Complete the following assessment in the Shadow Health platform
Complete the following assessment in the Shadow Health platform: Health History (180 mins.) including ROS
Health History
Effective communication is vital to constructing an accurate and detailed patient history. A patient’s health or illness is influenced by many factors, including age, gender, ethnicity, and environmental setting. As an advanced practice nurse, you must be aware of these factors and tailor your communication techniques accordingly. Doing so will not only help you establish rapport with your patients, but it will also enable you to more effectively gather the information needed to assess your patients’ health risks.
For this Assignment, you are introduced to Tina Jones, a virtual patient in the Shadow Health platform for which you will conduct an interactive health assessment. You will also practice effective communication and documentation of your findings.
To prepare:
- Review this week’s Resources and consider how you might incorporate these strategies into an effective health history. Download and review the Shadow Health Nursing Documentation Tutorial.
- Access and log in to Shadow Health using the link in the Start Here module of the Canvas classroom.
- Review the Shadow Health Student Orientation media program provided in the week’s Resources to guide you through Shadow Health.
- Review the Week 1 Assignment Rubric for details on Assignment expectations.
- Complete the following assessment in the Shadow Health platform:
- Health History (180 mins.) including ROS
- Sign, scan, and submit your Student Acknowledgement Form.
Note: Each Shadow Health Assessment may be reopened as many times as necessary prior to the due date to make documentation adjustments in order to achieve 80% or better, but you must make all edits to your documentation for the Health History by the Week 1 Day 7 deadline. It is recommended that you attempt it by no later than Day 5 in order to allow yourself enough time to familiarize yourself with Shadow Health and make any documentation edits by Day 7.
Expert Answer and Explanation
NURS 6380: Shadow Health
Week 1 Health History Exam Grading Rubric
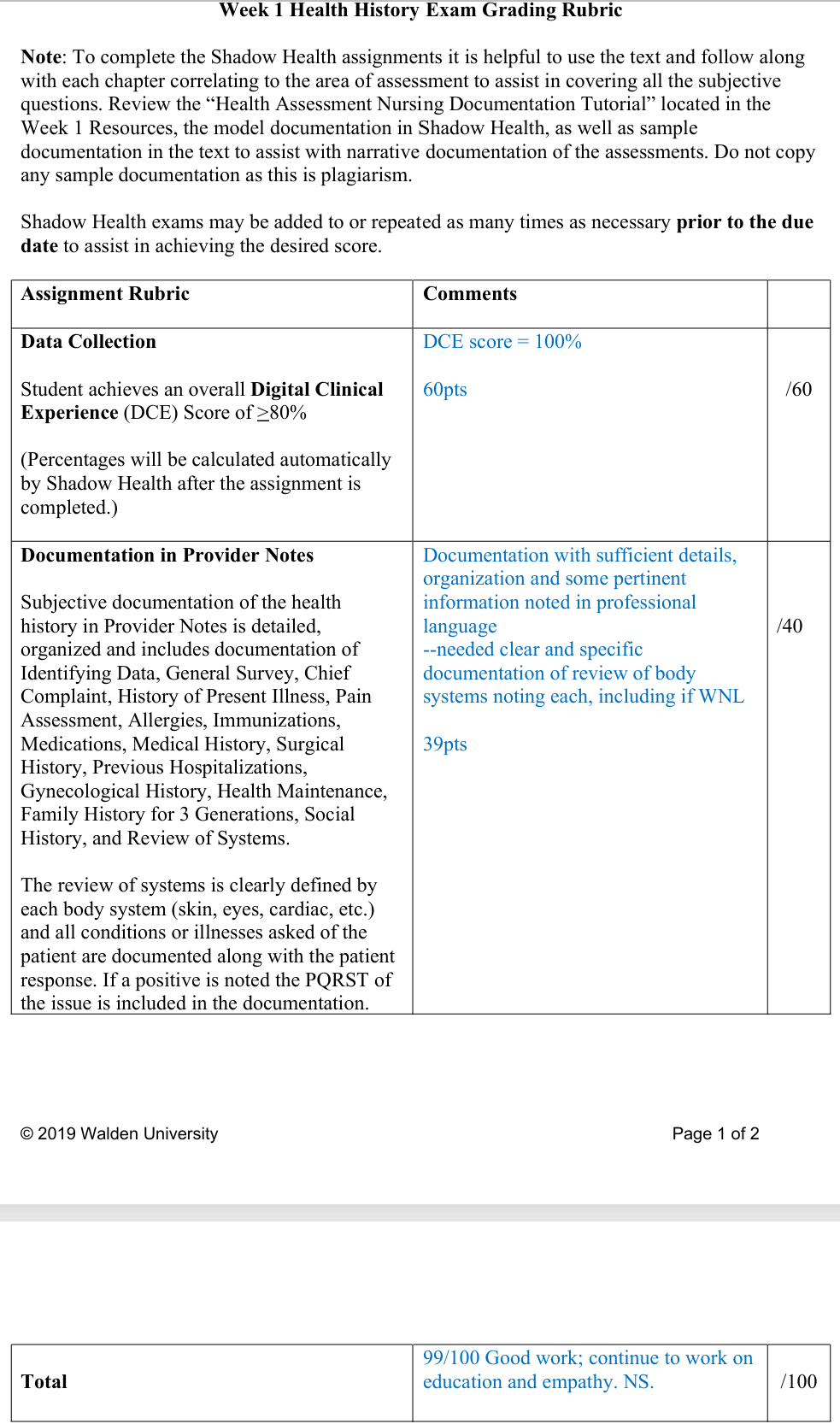
| Assignment Rubric | Comments |
|
| Data Collection
Student achieves an overall Digital Clinical Experience (DCE) Score of >80% (Percentages will be calculated automatically by Shadow Health after the assignment is completed.) |
DCE score = 100%
60pts |
/60 |
| Documentation in Provider Notes
Subjective documentation of the health history in Provider Notes is detailed, organized and includes documentation of Identifying Data, General Survey, Chief Complaint, History of Present Illness, Pain Assessment, Allergies, Immunizations, Medications, Medical History, Surgical History, Previous Hospitalizations, Gynecological History, Health Maintenance, Family History for 3 Generations, Social History, and Review of Systems. The review of systems is clearly defined by each body system (skin, eyes, cardiac, etc.) and all conditions or illnesses asked of the patient are documented along with the patient response. If a positive is noted the PQRST of the issue is included in the documentation. |
Documentation with sufficient details, organization and some pertinent information noted in professional language
–needed clear and specific documentation of review of body systems noting each, including if WNL 39pts |
/40 |
| Total | 99/100 Good work; continue to work on education and empathy. NS. |
/100 |
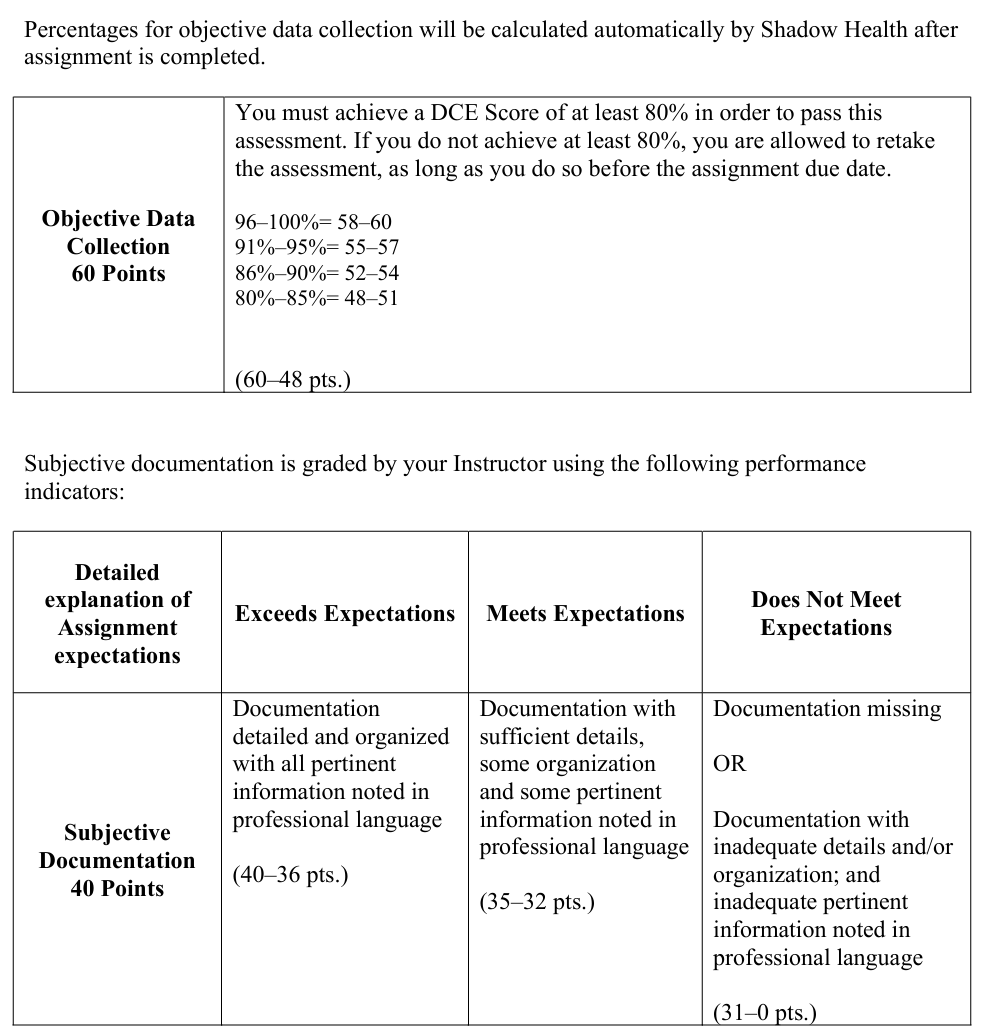
Percentages for objective data collection will be calculated automatically by Shadow Health after assignment is completed.
| Objective Data Collection
60 Points |
You must achieve a DCE Score of at least 80% in order to pass this assessment. If you do not achieve at least 80%, you are allowed to retake the assessment, as long as you do so before the assignment due date.
96–100%= 58–60 91%–95%= 55–57 86%–90%= 52–54 80%–85%= 48–51 (60–48 pts.) |
Subjective documentation is graded by your Instructor using the following performance indicators:
| Detailed explanation of Assignment expectations | Exceeds Expectations | Meets Expectations | Does Not Meet Expectations |
| Subjective Documentation
40 Points |
Documentation detailed and organized with all pertinent information noted in professional language
(40–36 pts.) |
Documentation with sufficient details, some organization and some pertinent information noted in professional language
(35–32 pts.) |
Documentation missing
OR Documentation with inadequate details and/or organization; and inadequate pertinent information noted in professional language (31–0 pts.) |
Place your order now for a similar assignment and get fast, affordable and best quality work written by our expert level assignment writers. Limited Offer: Use Coupon Code NEW30 to Get 30% OFF Your First Order
Limited Offer: Use Coupon Code NEW30 to Get 30% OFF Your First Order

How to Perform a Health Assessment in Nursing
Health assessments form the cornerstone of quality nursing practice, serving as the foundation for effective patient care and clinical decision-making (Potter et al., 2021). Whether you’re a nursing student preparing for clinical rotations or an experienced nurse looking to refine your assessment skills, understanding the intricacies of comprehensive health evaluations is essential for delivering optimal patient outcomes.
A thorough health assessment enables nurses to identify patient needs, detect early warning signs of health complications, and develop individualized care plans that address both immediate concerns and long-term wellness goals (Jarvis et al., 2019). This systematic approach to patient evaluation combines clinical expertise with evidence-based practices to ensure comprehensive, holistic care delivery (Institute of Medicine, 2010).
Health assessments form the cornerstone of quality nursing practice, serving as the foundation for effective patient care and clinical decision-making (Potter et al., 2021). Whether you’re a nursing student preparing for clinical rotations or an experienced nurse looking to refine your assessment skills, understanding the intricacies of comprehensive health evaluations is essential for delivering optimal patient outcomes.
A thorough health assessment enables nurses to identify patient needs, detect early warning signs of health complications, and develop individualized care plans that address both immediate concerns and long-term wellness goals (Jarvis et al., 2019). This systematic approach to patient evaluation combines clinical expertise with evidence-based practices to ensure comprehensive, holistic care delivery (Institute of Medicine, 2010).
Why Are Health Assessments Important in Nursing Practice?
Health assessments serve multiple critical functions within the healthcare system, acting as both diagnostic tools and preventive measures that significantly impact patient outcomes and overall healthcare quality.
Foundation for Clinical Decision-Making
Health assessments provide nurses with essential baseline data that informs all subsequent clinical decisions throughout a patient’s care journey (Weber & Kelley, 2018). This comprehensive evaluation process enables healthcare professionals to identify immediate health concerns, recognize potential complications before they become critical, and establish priority interventions based on evidence-based findings (Quality and Safety Education for Nurses, 2020). Without accurate initial assessments, nurses cannot develop effective care plans or make informed decisions about patient treatment modifications.
The systematic collection of subjective and objective data during health assessments creates a complete picture of the patient’s current health status, medical history, and risk factors (Jarvis et al., 2019). This information becomes invaluable when coordinating care with other healthcare team members, ensuring continuity of care across different settings, and documenting patient progress over time.
Early Detection and Prevention
One of the most significant benefits of comprehensive health assessments lies in their ability to identify health issues in early stages when interventions are most effective and less costly (U.S. Department of Health and Human Services, 2021). Nurses trained in thorough assessment techniques can detect subtle changes in patient condition that might otherwise go unnoticed until they progress to more serious complications.
Regular health assessments enable healthcare providers to identify risk factors for chronic diseases, screen for common health conditions, and implement preventive measures that can significantly improve long-term patient outcomes (Institute of Medicine, 2010). This proactive approach to healthcare delivery not only benefits individual patients but also contributes to overall public health improvement and healthcare cost reduction.
Legal and Professional Standards
Health assessments fulfill important legal and professional requirements within nursing practice, serving as documented evidence of the nurse’s competency and adherence to established standards of care (National Council of State Boards of Nursing, 2024). Proper documentation of assessment findings protects both patients and healthcare providers while ensuring compliance with regulatory requirements and accreditation standards.
Professional nursing organizations and healthcare institutions mandate specific assessment protocols and documentation requirements that nurses must follow to maintain their licensure and professional standing (Potter et al., 2021). These standards ensure consistency in care delivery and provide frameworks for quality improvement initiatives within healthcare organizations.
Patient Safety and Quality Assurance
Comprehensive health assessments directly contribute to patient safety by identifying potential complications, medication interactions, and environmental hazards that could negatively impact patient outcomes (Aebersold et al., 2023). This systematic evaluation process helps prevent medical errors, reduces the risk of adverse events, and ensures appropriate resource allocation based on individual patient needs.
Quality assurance programs within healthcare organizations rely heavily on assessment data to monitor care effectiveness, identify areas for improvement, and implement evidence-based practice changes that enhance overall patient satisfaction and clinical outcomes (Thompson et al., 2023).
How Is a Health Assessment Performed in Nursing?
Performing a comprehensive health assessment requires systematic organization, clinical expertise, and strong communication skills to gather accurate and complete information about the patient’s health status and care needs.
Pre-Assessment Preparation
Before beginning any health assessment, nurses must prepare both themselves and the environment to ensure optimal conditions for accurate data collection (Weber & Kelley, 2018). This preparation phase includes reviewing available medical records, gathering necessary assessment tools and equipment, and creating a comfortable, private environment that promotes open communication between the nurse and patient.
Essential equipment for comprehensive health assessments typically includes a stethoscope, blood pressure cuff, thermometer, penlight, measuring tape, reflex hammer, and appropriate forms for documentation (Jarvis et al., 2019). Nurses should also ensure they have adequate time allocated for the assessment process without interruptions that could compromise the quality of data collection.
Environmental considerations include proper lighting for visual inspections, comfortable room temperature, and privacy protection that allows patients to feel secure when sharing sensitive health information or during physical examination components of the assessment process (Potter et al., 2021).
Subjective Data Collection
The subjective portion of health assessment involves gathering information directly from the patient about their health concerns, symptoms, medical history, and personal experiences related to their current health status (U.S. Department of Health and Human Services, 2021). This phase requires excellent communication skills and active listening techniques to encourage patients to share comprehensive and accurate information.
Primary components of subjective data collection include obtaining a detailed health history, identifying the chief complaint or reason for seeking healthcare services, exploring the history of present illness with attention to symptom onset, duration, and associated factors, and reviewing past medical history including previous hospitalizations, surgeries, and chronic conditions (Jarvis et al., 2019).
Nurses must also gather information about family health history, social determinants of health including lifestyle factors and environmental exposures, current medications and supplements, known allergies and adverse reactions, and psychosocial factors that may impact health outcomes such as stress levels, support systems, and coping mechanisms (Weber & Kelley, 2018).
Objective Data Collection Through Physical Examination
The objective component of health assessment involves systematic physical examination using inspection, palpation, percussion, and auscultation techniques to gather measurable and observable data about the patient’s current physiological status and overall health condition (Potter et al., 2021).
Physical examination typically follows a head-to-toe approach, beginning with general appearance and vital signs assessment, followed by systematic evaluation of each body system (Jarvis et al., 2019). This includes cardiovascular assessment through heart rate, rhythm, and blood pressure monitoring, respiratory evaluation including lung sounds and breathing patterns, neurological examination testing reflexes, coordination, and cognitive function, and musculoskeletal assessment evaluating strength, range of motion, and functional capacity.
Additional objective data collection may include laboratory results, diagnostic imaging findings, and measurements such as height, weight, body mass index calculations, and specific assessments related to the patient’s presenting concerns or risk factors identified during the subjective data collection phase (Weber & Kelley, 2018).
Documentation and Analysis
Accurate documentation of assessment findings is crucial for communication with other healthcare team members, continuity of care, and legal protection for both patients and healthcare providers (National Council of State Boards of Nursing, 2024). Documentation should be thorough, objective, and organized in a standardized format that facilitates easy retrieval and interpretation of information.
Following data collection, nurses must analyze their findings to identify patterns, prioritize patient needs, and develop appropriate nursing diagnoses and care plans (Quality and Safety Education for Nurses, 2020). This analysis process requires critical thinking skills and the ability to synthesize subjective and objective data into meaningful conclusions that guide subsequent nursing interventions and care planning decisions.
How Do Nurses Learn to Perform Health Assessments?
Learning to perform comprehensive health assessments is a progressive process that combines theoretical knowledge, practical skills development, and ongoing professional education throughout a nurse’s career.
Academic Foundation in Nursing Education
Nursing education programs provide the foundational knowledge and skills necessary for competent health assessment performance through structured coursework and clinical experiences (Benner et al., 2010). Students typically begin with anatomy and physiology courses that provide essential understanding of normal body structure and function, followed by pathophysiology courses that explain disease processes and abnormal findings.
Dedicated health assessment courses teach students systematic examination techniques, proper use of assessment equipment, normal versus abnormal finding identification, and documentation requirements (Rossetti & Fox, 2009). These courses typically combine classroom instruction with laboratory practice sessions where students can develop and refine their technical skills before applying them in clinical settings with actual patients.
Simulation-based learning experiences allow nursing students to practice assessment skills in controlled environments where mistakes can be learning opportunities without patient safety concerns (Cant & Cooper, 2017). High-fidelity mannequins and standardized patients provide realistic scenarios that help students develop confidence and competency before transitioning to actual patient care environments (Hayden et al., 2014).
Clinical Practice and Mentorship
Hands-on clinical experience under the supervision of experienced nurses and clinical instructors is essential for developing proficiency in health assessment performance (Zhou et al., 2024). These supervised practice opportunities allow students to apply theoretical knowledge in real-world settings while receiving immediate feedback and guidance from experienced professionals.
Mentorship relationships between experienced nurses and novice practitioners provide ongoing support and skill development opportunities that extend beyond formal education programs (Rossetti & Fox, 2009). These relationships offer personalized guidance, professional role modeling, and continuous learning opportunities that help new nurses refine their assessment skills and develop clinical judgment capabilities.
Clinical rotations across various healthcare settings expose nursing students to diverse patient populations and health conditions, broadening their assessment experience and helping them develop adaptability in their approach to different patient needs and clinical environments (Johnson et al., 2024).
Continuing Education and Professional Development
Professional nursing practice requires ongoing education and skill development to maintain competency and stay current with evolving best practices in health assessment techniques and technologies (National Council of State Boards of Nursing, 2024). Many healthcare organizations provide regular training programs, workshops, and competency validation processes to ensure their nursing staff maintain high standards of assessment performance.
Professional nursing organizations offer continuing education opportunities, certification programs, and specialty training courses that help nurses develop advanced assessment skills in specific areas of practice such as cardiac assessment, neurological evaluation, or pediatric health assessment techniques (Institute of Medicine, 2010).
Peer learning opportunities through professional conferences, journal clubs, and collaborative practice initiatives provide valuable forums for sharing knowledge, discussing challenging cases, and learning from colleagues’ experiences in health assessment performance and interpretation (Chen et al., 2023).
Technology Integration and Modern Assessment Tools
Contemporary nursing education increasingly incorporates technology-enhanced learning tools and electronic health assessment documentation systems that reflect current healthcare practice environments (Giddens, 2008). Students learn to use electronic health records, mobile assessment applications, and digital monitoring devices that are standard in modern healthcare settings.
Telehealth and remote assessment capabilities are becoming increasingly important components of nursing education as healthcare delivery models evolve to include virtual care options (Zhang et al., 2023). Nurses must develop skills in conducting health assessments through technology platforms while maintaining the same standards of thoroughness and accuracy as traditional in-person evaluations.
Advanced simulation technologies and virtual reality platforms provide innovative learning opportunities that allow students to practice complex assessment scenarios and develop critical thinking skills in safe, controlled environments (Park et al., 2023). These technologies supplement traditional clinical experiences and help prepare nurses for the increasingly complex healthcare environments they will encounter in professional practice.
Conclusion: Mastering Health Assessment Skills for Optimal Patient Care
Health assessment represents a fundamental competency that distinguishes professional nursing practice and directly impacts patient outcomes across all healthcare settings (Potter et al., 2021). The systematic approach to gathering, analyzing, and documenting patient health information provides the foundation for safe, effective, and individualized patient care that addresses both immediate needs and long-term wellness goals.
Successful health assessment performance requires ongoing commitment to professional development, continuous learning, and practice refinement throughout a nurse’s career (González-García et al., 2023). As healthcare continues to evolve with new technologies, changing patient demographics, and emerging health challenges, nurses must remain adaptable and committed to maintaining their assessment skills at the highest professional standards.
The investment in developing comprehensive health assessment competencies pays dividends throughout a nursing career, enhancing clinical decision-making capabilities, improving patient satisfaction, and contributing to overall healthcare quality improvement initiatives (Aebersold et al., 2023). Whether working in acute care hospitals, community health settings, or specialized practice environments, nurses who excel in health assessment provide invaluable contributions to their healthcare teams and the patients they serve.
References
- Aebersold, M., Tschannen, D., & Bathish, M. (2023). Effects of implementation strategies on nursing practice and patient outcomes: A comprehensive systematic review and meta-analysis. Implementation Science, 19(1), 1-15.
- Azer, S. A., Guerrero, A. P., & Walsh, A. (2013). Enhancing learning approaches: Practical tips for students and teachers. Medical Teacher, 35(6), 433-443.
- Benner, P., Sutphen, M., Leonard, V., & Day, L. (2010). Educating nurses: A call for radical transformation. Jossey-Bass.
- Cant, R. P., & Cooper, S. J. (2017). Use of simulation-based learning in undergraduate nurse education: An umbrella systematic review. Nurse Education Today, 49, 63-71.
- Chen, L., Wang, X., & Liu, Y. (2023). Effects of simulation in improving the self-confidence of student nurses in clinical practice: A systematic review. BMC Medical Education, 23(1), 798.
- Foronda, C., Liu, S., & Bauman, E. B. (2013). Evaluation of simulation in undergraduate nurse education: An integrative review. Clinical Simulation in Nursing, 9(10), e409-e416.
- Giddens, J. F. (2008). The neighborhood: A web-based platform to support conceptual teaching and learning. Nursing Education Perspectives, 29(5), 251-256.
- González-García, A., Martínez-López, B., & Rodríguez-Pérez, C. (2023). Comparing formative and summative simulation-based assessment in undergraduate nursing students: Nursing competency acquisition and clinical simulation satisfaction. BMC Nursing, 22(1), 156.
- Hayden, J. K., Smiley, R. A., Alexander, M., Kardong-Edgren, S., & Jeffries, P. R. (2014). The NCSBN National Simulation Study: A longitudinal, randomized, controlled study replacing clinical hours with simulation in prelicensure nursing education. Journal of Nursing Regulation, 5(2), S3-S40.
- Institute of Medicine. (2010). The future of nursing: Leading change, advancing health. The National Academies Press.
- Jarvis, C., Browne, A. J., MacDonald-Jenkins, J., & Luctkar-Flude, M. (2019). Physical examination and health assessment (3rd Canadian ed.). Elsevier.
- Jeffries, P. R., & Rogers, K. J. (2012). Theoretical framework for simulation design. The National League for Nursing.
- Johnson, M., Smith, R., & Davis, K. (2024). Effectiveness of a simulation-based education program to improve novice nurses’ clinical judgment skills. Clinical Simulation in Nursing, 87, 45-52.
- National Council of State Boards of Nursing. (2024). The 2024 National Nursing Workforce Survey. Journal of Nursing Regulation, 15(2), S1-S48.
- Park, S., Kim, H., & Lee, J. (2023). Nursing students’ clinical judgment skills in simulation and clinical placement: A comparison of student self-assessment and evaluator assessment. BMC Nursing, 22(1), 243.
- Potter, P. A., Perry, A. G., Stockert, P. A., & Hall, A. M. (2021). Fundamentals of nursing (10th ed.). Elsevier.
- Quality and Safety Education for Nurses. (2020). QSEN competencies. Retrieved from http://qsen.org/competencies/
- Rossetti, J., & Fox, P. G. (2009). Factors related to successful teaching by outstanding professors: An interpretive study. Journal of Nursing Education, 48(1), 11-16.
- Rutherford-Hemming, T. (2012). Simulation methodology in nursing education and adult learning theory. Adult Learning, 23(3), 129-137.
- Shin, S., Park, J. H., & Kim, J. H. (2015). Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Education Today, 35(1), 176-182.
- Thompson, A., Wilson, B., & Anderson, C. (2023). High-fidelity simulation’s impact on clinical reasoning and patient safety: A scoping review. Journal of Nursing Regulation, 14(3), 24-35.
- U.S. Department of Health and Human Services. (2021). Nursing admission assessment and examination. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK493211/
- Weber, J. R., & Kelley, J. H. (2018). Health assessment in nursing (6th ed.). Lippincott Williams & Wilkins.
- Zhang, P., Li, M., & Wang, H. (2023). Simulation-based learning in nursing curriculum – Time to prepare quality nurses: A systematic review and meta-analysis. International Journal of Nursing Sciences, 10(3), 287-297.
- Zhou, X., Brown, L., & Taylor, S. (2024). Learning clinical skills in the simulation suite: The lived experiences of student nurses involved in peer teaching and peer assessment. Nurse Education in Practice, 75, 103-112.
Required Readings

Dan Palmer is a dedicated academic writing specialist with extensive experience supporting nursing students throughout their educational journey. Understanding the unique challenges faced by nursing students who balance demanding clinical rotations, family responsibilities, and rigorous coursework, Dan provides professional assignment assistance that helps students maintain academic excellence without compromising their other commitments.
With a comprehensive understanding of nursing curriculum requirements and academic standards, Dan delivers high-quality, thoroughly researched assignments that serve as valuable learning resources. His expertise spans various nursing disciplines, including clinical practice, healthcare ethics, patient care management, and evidence-based research.
Dan’s approach combines meticulous attention to detail with a commitment to timely delivery, ensuring that busy nursing students receive the support they need when they need it most. His professional assistance has helped countless nursing students successfully navigate their academic programs while maintaining their professional and personal responsibilities.
Committed to academic integrity and excellence, Dan Palmer continues to be a trusted resource for nursing students seeking reliable, professional assignment support.


