Complete the following in Shadow Health, depending on which patient you selected for your first focused exam
Complete the following in Shadow Health, depending on which patient you selected for your first focused exam
Focused Exam 1
It is crucial to diagnose cardiac and respiratory conditions early due to the critical nature of these organs. Before a condition can be diagnosed, an examination must be conducted. Properly conducting cardiac and respiratory examinations requires detailed knowledge of the examination procedure and experience in performing these assessments.
For this Assignment, and the next assignment, you will perform virtual focused exams in Shadow Health on the respiratory and cardiovascular systems.
Resources
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
To prepare:
- Review this week’s Resources, with particular attention to the relevant Bickley (2024) chapter for each body system addressed in the Assignments this week.
- Review the Week 2 Shadow Health Focused Exam Rubric provided in the Course Information area for details on completing the Assignment in Shadow Health.
- Select either the patient Brian or Danny to focus on for your first focused exam.
- Explore the concept lab related to your patient’s system of concern before completing the physical exam.
- Complete the following in Shadow Health, depending on which patient you selected for your first focused exam:
- Respiratory Concept Lab (Recommended but not required)
- Focused Exam: Cough (90 mins.)
OR - Cardiovascular Concept Lab (Recommended but not required)
- Abdominal Concept Lab (Recommended but not required)
- Focused Exam: Chest Pain (90 mins.)
- Sign, scan, and submit your Student Acknowledgement Form.
Note: Each Shadow Health Assessment may be reopened as many times as necessary prior to the due date to make documentation adjustments in order to achieve 80% or better, but you must make all edits to your documentation for the first Focused Exam by the Week 2 Day 3 deadline.
Submit your Assignment in Shadow Health by Day 3.
Expert Answer and Explanation
NURS 6380: Shadow Health
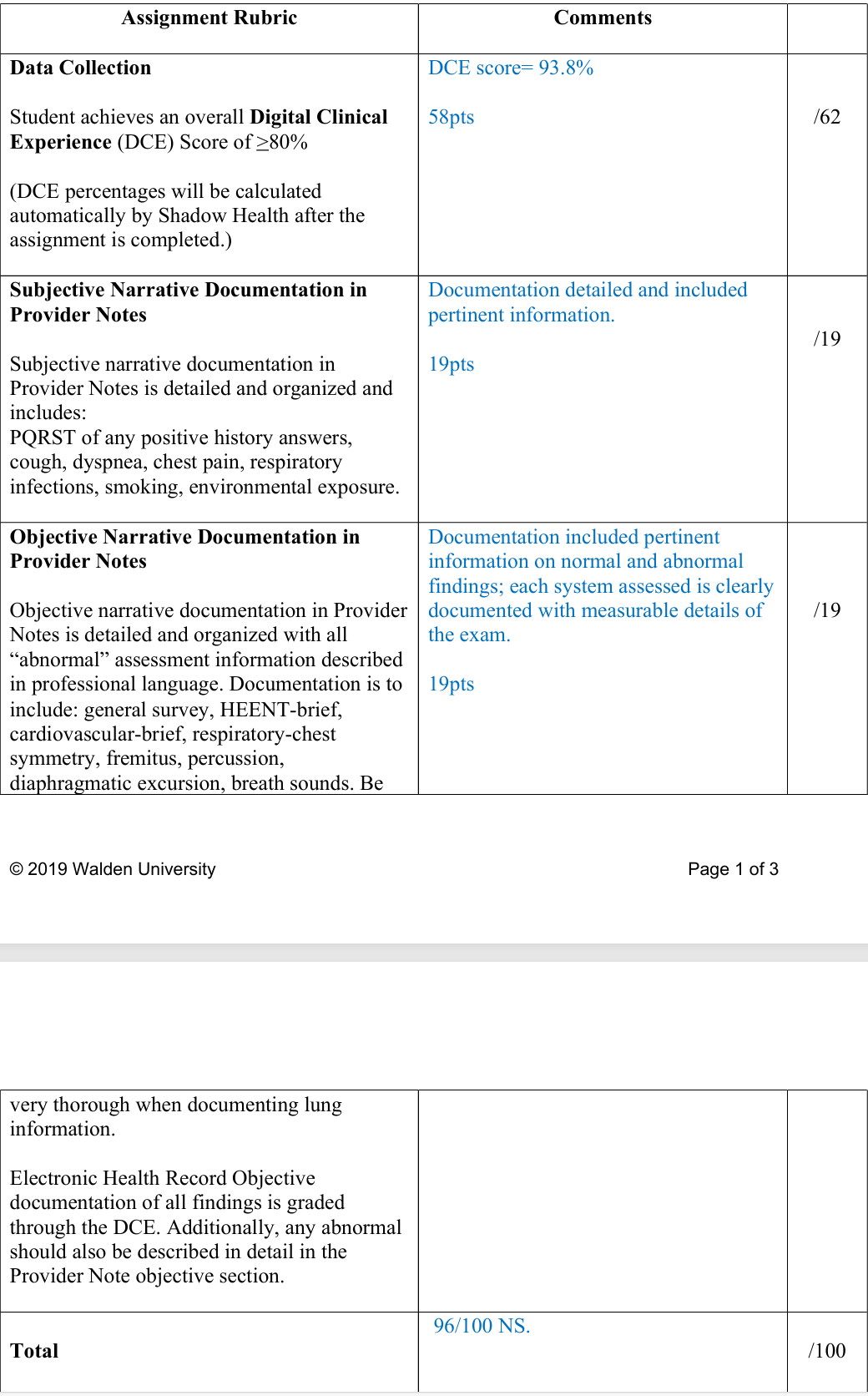
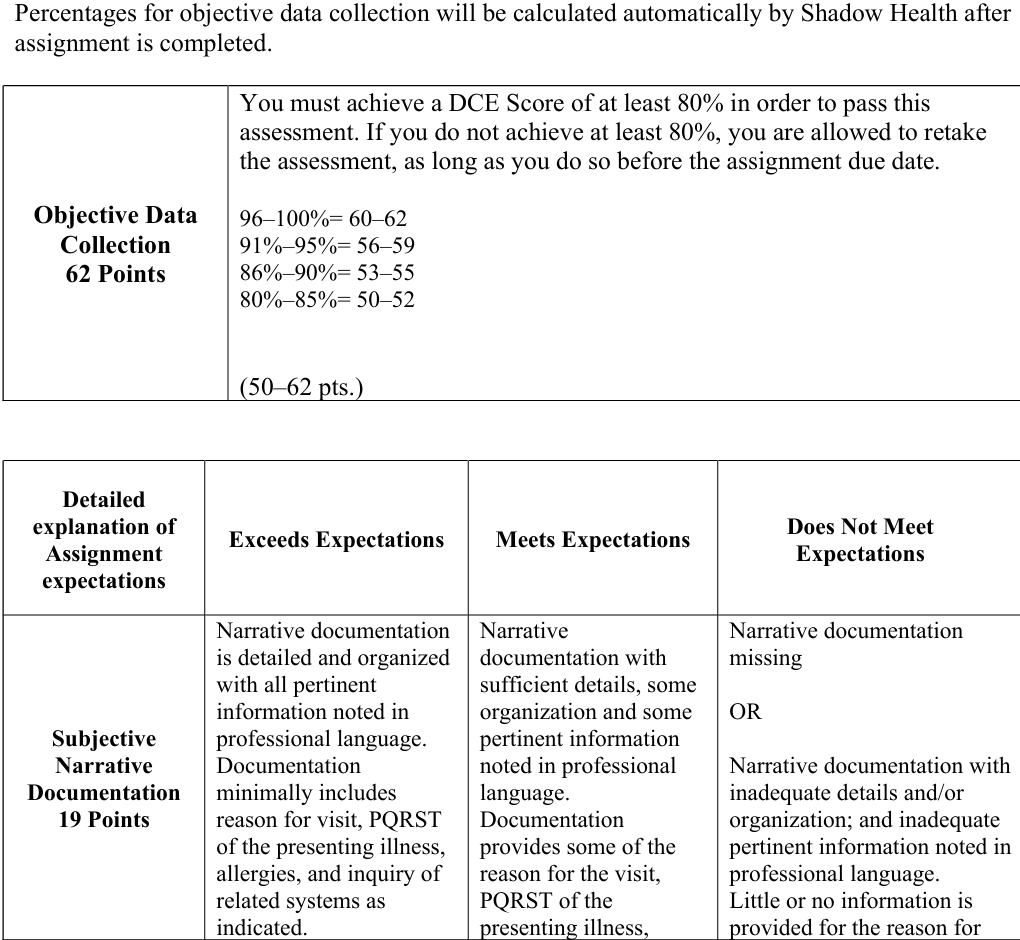
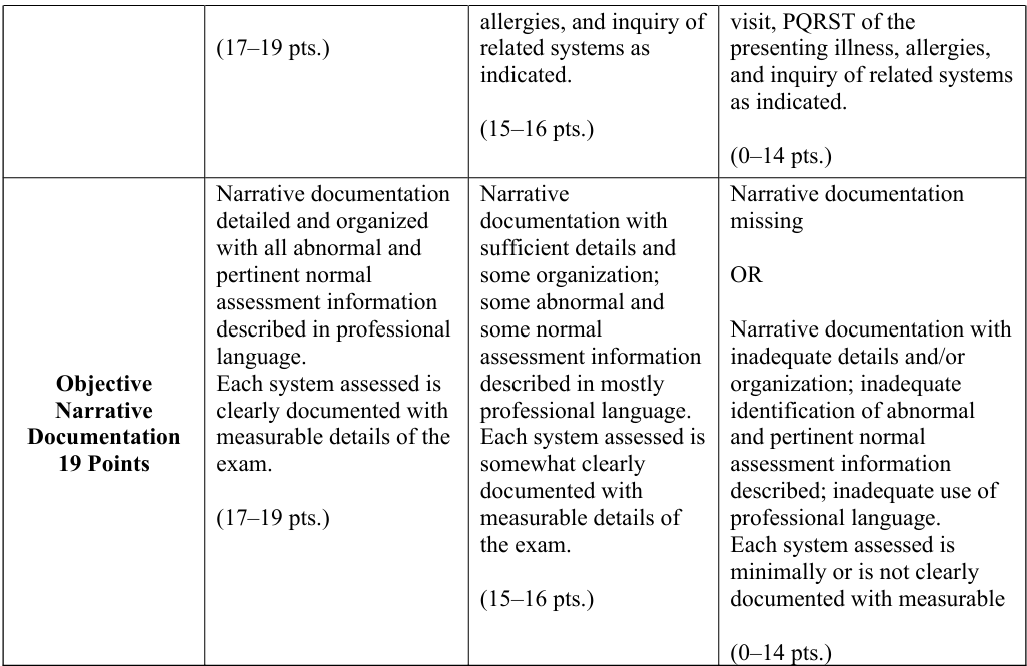
Week 2: Respiratory Focused Exam Grading Rubric
To complete the Shadow Health assignments, it is helpful to use the text and follow along with each chapter correlating to the area of assessment to assist in covering all the subjective questions and the physical assessment areas. Review the “Health Assessment Nursing Documentation Tutorial” located in the Week 1 Resources, the model documentation in Shadow Health, as well as sample documentation in the text to assist with narrative documentation of the assessments. Do not copy any sample documentation as this is plagiarism.
Shadow Health exams may be added to or repeated as many times as necessary prior to the due date to assist in achieving the desired score.
Place your order now for a similar assignment and get fast, affordable and best quality work written by our expert level assignment writers. Limited Offer: Use Coupon Code NEW30 to Get 30% OFF Your First Order
Limited Offer: Use Coupon Code NEW30 to Get 30% OFF Your First Order

Head-to-Toe Assessment in Nursing
What Is a Head-to-Toe Assessment?
A head-to-toe assessment is a comprehensive, systematic physical examination that nurses perform to evaluate a patient’s overall health status. This thorough evaluation involves inspecting, palpating, percussing, and auscultating every body system from the patient’s head down to their toes. The assessment provides baseline data, identifies potential health problems, monitors changes in condition, and guides nursing interventions.
The head-to-toe assessment follows a logical sequence that ensures no body system is overlooked while maintaining patient comfort and dignity. It combines objective data collection through physical examination techniques with subjective information gathered from patient interviews.
When Is a Head-to-Toe Assessment Typically Performed?
Head-to-toe assessments are performed in various clinical situations:
Routine Situations:
- Hospital admissions to establish baseline data
- Beginning of each nursing shift in acute care settings
- Pre-operative evaluations
- Annual physical examinations in outpatient settings
- Long-term care facility admissions
Urgent Situations:
- When patients report new symptoms or complaints
- Following significant changes in patient condition
- After medical procedures or interventions
- When vital signs indicate potential problems
- Emergency department presentations
Monitoring Situations:
- Post-operative recovery periods
- During medication administration that requires monitoring
- When patients have chronic conditions requiring regular assessment
- Before discharge planning
Initial Assessment Steps
Before beginning the physical examination, several preparatory steps ensure an effective and professional assessment:
Environmental Preparation:
- Ensure adequate lighting and privacy
- Gather necessary equipment (stethoscope, thermometer, blood pressure cuff, penlight, etc.)
- Maintain comfortable room temperature
- Remove potential distractions
Patient Preparation:
- Introduce yourself and explain the assessment process
- Obtain informed consent
- Position the patient appropriately
- Ensure patient comfort and dignity
- Wash hands and don appropriate personal protective equipment
Initial Data Collection:
- Review medical history and current medications
- Obtain vital signs (temperature, pulse, respirations, blood pressure, oxygen saturation, pain level)
- Conduct brief patient interview about current concerns
- Assess level of consciousness and orientation
Head-to-Toe Assessment Checklist
Head and Neck Assessment
General Appearance:
- Overall appearance and grooming
- Facial expressions and symmetry
- Skin color, temperature, and moisture
- Evidence of distress or discomfort
Head:
- Inspect scalp for lesions, masses, or tenderness
- Assess hair texture, distribution, and cleanliness
- Examine facial features for symmetry
- Check temporal arteries for tenderness or enlargement
Eyes:
- Inspect eyelids for swelling, drooping, or lesions
- Assess pupil size, shape, and reaction to light
- Test extraocular movements
- Examine conjunctiva and sclera
- Assess visual acuity if indicated
Ears:
- Inspect external ears for deformities or discharge
- Assess hearing ability
- Examine ear canals with otoscope if trained
- Palpate mastoid process for tenderness
Nose:
- Inspect external nose for deformities
- Check nasal passages for obstruction or discharge
- Assess sense of smell if indicated
- Palpate sinuses for tenderness
Mouth and Throat:
- Inspect lips for color, moisture, and lesions
- Examine teeth and gums for condition
- Assess tongue color, texture, and movement
- Inspect throat and tonsils
- Evaluate speech clarity and voice quality
Neck:
- Inspect for masses, swelling, or asymmetry
- Palpate lymph nodes systematically
- Assess neck range of motion
- Palpate thyroid gland
- Inspect and palpate carotid arteries
Chest and Respiratory Assessment
Inspection:
- Observe chest shape, symmetry, and movement
- Note breathing pattern and effort
- Assess use of accessory muscles
- Check for retractions or abnormal movements
Palpation:
- Feel for masses, tenderness, or crepitus
- Assess chest expansion
- Palpate for fremitus
Percussion:
- Percuss lung fields systematically
- Note resonance patterns
Auscultation:
- Listen to breath sounds in all lung fields
- Identify normal and abnormal sounds
- Assess for adventitious sounds (crackles, wheezes, rhonchi)
Cardiovascular Assessment
Inspection:
- Observe for visible pulsations
- Note skin color and perfusion
- Assess for edema or swelling
Palpation:
- Feel for point of maximal impulse
- Assess peripheral pulses (radial, brachial, carotid, femoral, posterior tibial, dorsalis pedis)
- Check capillary refill time
Auscultation:
- Listen to heart sounds in all four areas
- Identify S1 and S2 sounds
- Note any murmurs, gallops, or extra sounds
- Assess heart rate and rhythm
Abdominal Assessment
Inspection:
- Observe abdominal shape, symmetry, and movement
- Note skin color and any visible masses
- Check for distension or abnormal pulsations
Auscultation (performed before palpation):
- Listen to bowel sounds in all four quadrants
- Assess frequency and character of sounds
- Listen for bruits over major vessels
Percussion:
- Percuss all four quadrants
- Assess liver span
- Check for fluid wave if ascites suspected
Palpation:
- Begin with light palpation in all quadrants
- Progress to deep palpation if appropriate
- Assess for masses, tenderness, or organ enlargement
- Palpate specific organs (liver, spleen, kidneys)
Genitourinary Assessment
General:
- Inspect external genitalia for abnormalities
- Assess for discharge, lesions, or swelling
- Note urinary patterns and concerns
Male-Specific:
- Inspect penis and scrotum
- Palpate testes if indicated
- Assess for hernias
Female-Specific:
- Inspect external genitalia
- Note menstrual history if relevant
- Assess for prolapse or discharge
Musculoskeletal Assessment
Inspection:
- Observe posture and gait
- Note muscle mass and symmetry
- Assess for deformities or swelling
- Check alignment of extremities
Palpation:
- Feel for muscle tone and strength
- Assess joints for swelling, warmth, or tenderness
- Check for crepitus in joints
Range of Motion:
- Test active and passive range of motion
- Assess flexibility and limitations
- Note any pain with movement
Strength Testing:
- Evaluate muscle strength systematically
- Use standardized grading scale (0-5)
- Test major muscle groups
Neurological Assessment
Mental Status:
- Assess level of consciousness
- Evaluate orientation (person, place, time, situation)
- Test memory and cognitive function
- Assess mood and affect
Cranial Nerves:
- Test all 12 cranial nerves systematically
- Note any deficits or abnormalities
Motor Function:
- Assess muscle strength and tone
- Test coordination and balance
- Evaluate gait and posture
Sensory Function:
- Test light touch, deep pressure, and pain sensation
- Assess temperature sensation if indicated
- Check proprioception and vibration
Reflexes:
- Test deep tendon reflexes
- Assess superficial reflexes
- Note symmetry and response quality
Skin and Integumentary Assessment
Inspection:
- Observe overall skin color and tone
- Note any lesions, rashes, or discoloration
- Assess hair and nail condition
- Check for pressure areas or wounds
Palpation:
- Feel skin temperature and moisture
- Assess skin turgor and elasticity
- Palpate any lesions or masses
- Check capillary refill
Head-to-Toe Assessment Checklist Template
Patient Information
- Name: ________________
- Date: ________________
- Time: ________________
- Nurse: ________________
Vital Signs
- Temperature: ______°F/°C
- Pulse: ______ bpm
- Respirations: ______ per minute
- Blood Pressure: / mmHg
- Oxygen Saturation: ______%
- Pain Level: ______/10
General Appearance
- [ ] Alert and oriented x4
- [ ] Appears comfortable
- [ ] No acute distress
- [ ] Appropriate grooming
- Notes: ________________
Head and Neck
- [ ] Head normocephalic
- [ ] Pupils equal, round, reactive to light
- [ ] Extraocular movements intact
- [ ] Hearing grossly intact
- [ ] Nose patent bilaterally
- [ ] Oral mucosa pink and moist
- [ ] Neck supple, no lymphadenopathy
- Abnormal findings: ________________
Respiratory
- [ ] Chest rises symmetrically
- [ ] Breathing unlabored
- [ ] Clear breath sounds bilaterally
- [ ] No adventitious sounds
- [ ] No use of accessory muscles
- Abnormal findings: ________________
Cardiovascular
- [ ] Regular rate and rhythm
- [ ] S1 and S2 present
- [ ] No murmurs/gallops/rubs
- [ ] Peripheral pulses present and equal
- [ ] Capillary refill <3 seconds
- [ ] No peripheral edema
- Abnormal findings: ________________
Abdominal
- [ ] Soft, non-tender, non-distended
- [ ] Bowel sounds present x4 quadrants
- [ ] No masses palpated
- [ ] No organomegaly
- Abnormal findings: ________________
Genitourinary
- [ ] No abnormalities noted
- [ ] Continent of urine
- [ ] No discharge or lesions
- Abnormal findings: ________________
Musculoskeletal
- [ ] Full range of motion
- [ ] Muscle strength 5/5 bilaterally
- [ ] Steady gait
- [ ] No joint swelling or deformity
- Abnormal findings: ________________
Neurological
- [ ] Alert and oriented
- [ ] Speech clear and appropriate
- [ ] Motor function intact
- [ ] Sensation intact
- [ ] Reflexes 2+ and symmetric
- Abnormal findings: ________________
Skin/Integumentary
- [ ] Skin warm, dry, intact
- [ ] Good skin turgor
- [ ] No lesions or rashes
- [ ] Nails pink with good capillary refill
- Abnormal findings: ________________
What Are the 4 Types of Nursing Assessment?
Nursing assessments are categorized into four distinct types, each serving specific purposes in patient care:
1. Initial Assessment (Comprehensive Assessment)
This is the most thorough type of assessment performed when a patient first enters the healthcare system or at the beginning of care. It establishes a complete baseline of the patient’s health status.
Characteristics:
- Comprehensive health history collection
- Complete physical examination
- Psychosocial assessment
- Assessment of all body systems
- Identification of patient’s needs and problems
- Development of nursing diagnoses
When performed:
- Hospital admissions
- First clinic visits
- Beginning of home health care
- Long-term care facility admissions
2. Focused Assessment (Problem-Focused Assessment)
This assessment concentrates on specific problems, symptoms, or body systems. It’s more limited in scope but detailed in the area of concern.
Characteristics:
- Targets specific complaints or problems
- Concentrates on related body systems
- Uses detailed examination techniques for the problem area
- Builds upon previous assessment data
When performed:
- Patient reports new symptoms
- Changes in condition occur
- Follow-up on known problems
- Pre- and post-procedure monitoring
3. Ongoing Assessment (Partial Assessment)
This type involves continuous monitoring and evaluation of the patient’s condition and response to treatments.
Characteristics:
- Regular monitoring of specific parameters
- Assessment of response to interventions
- Comparison with previous findings
- Documentation of changes over time
When performed:
- Shift assessments
- Medication administration checks
- Routine monitoring
- Progress evaluations
4. Emergency Assessment
This rapid assessment focuses on identifying life-threatening conditions and prioritizing immediate interventions.
Characteristics:
- Quick identification of critical issues
- Prioritization based on urgency
- Focus on airway, breathing, circulation
- Minimal but essential data collection
When performed:
- Emergency situations
- Rapid response calls
- Code situations
- Acute deterioration
What Are the 5 P’s of Nursing Assessment?
The 5 P’s represent a systematic approach to patient assessment that ensures comprehensive evaluation and helps prioritize care:
1. Pain
Pain assessment is considered the fifth vital sign and requires thorough evaluation.
Assessment components:
- Location and radiation of pain
- Quality and character of pain
- Intensity using appropriate scales (0-10, faces, behavioral)
- Timing and duration
- Precipitating and alleviating factors
- Patient’s response to pain management
2. Potty (Elimination)
Assessment of urinary and bowel elimination patterns is crucial for identifying problems and planning care.
Urinary assessment:
- Frequency, urgency, and volume
- Color, clarity, and odor
- Incontinence issues
- Presence of catheters
Bowel assessment:
- Frequency and consistency of bowel movements
- Last bowel movement
- Presence of constipation or diarrhea
- Abdominal distension or discomfort
3. Position (Mobility and Safety)
Evaluation of patient’s ability to move safely and maintain proper positioning.
Assessment areas:
- Mobility level and limitations
- Fall risk factors
- Need for assistive devices
- Positioning needs for comfort and safety
- Skin integrity related to positioning
4. Periphery (Circulation)
Assessment of peripheral circulation and neurovascular status.
Components:
- Peripheral pulses
- Skin color, temperature, and capillary refill
- Presence of edema
- Sensation and movement in extremities
- Signs of compromised circulation
5. Psychological/Psychosocial
Evaluation of mental health, emotional status, and social factors affecting health.
Assessment includes:
- Mental status and orientation
- Mood and affect
- Anxiety or depression screening
- Coping mechanisms
- Support systems
- Cultural considerations
Examples of Nursing Assessments
Example of a Complete Nursing Assessment
Patient: 65-year-old male admitted with chest pain
Chief Complaint: “I’ve been having chest pain for the past 2 hours that feels like pressure and radiates to my left arm.”
Assessment Findings:
- Vital Signs: T: 98.6°F, P: 102 bpm, R: 22/min, BP: 160/95 mmHg, O2 Sat: 94% on room air, Pain: 7/10
- General: Alert, oriented, appears anxious and in moderate distress
- Cardiovascular: Tachycardic, regular rhythm, no murmurs, peripheral pulses present
- Respiratory: Slight tachypnea, lungs clear bilaterally, no shortness of breath at rest
- Neurological: Alert and oriented x4, no focal deficits
- Skin: Diaphoretic, color pale
- Pain: Substernal chest pressure, 7/10 intensity, radiates to left arm
Nursing Diagnoses:
- Acute pain related to myocardial ischemia
- Anxiety related to chest pain and fear of heart attack
- Risk for decreased cardiac output
Example of a Focused Assessment
Situation: Post-operative patient day 1 after abdominal surgery, reports increased abdominal pain
Focused Abdominal Assessment:
- Pain: Increased from 4/10 to 8/10, sharp, localized to incision site
- Inspection: Surgical dressing dry and intact, slight abdominal distension
- Auscultation: Bowel sounds hypoactive in all quadrants
- Palpation: Incision tender to palpation, no masses felt, bladder not distended
- Vital Signs: T: 100.2°F, P: 95 bpm, BP: 135/80 mmHg (baseline: T: 98.6°F, P: 78 bpm, BP: 120/70 mmHg)
Assessment: Possible complications include infection, ileus, or normal post-operative pain requiring reassessment and possible intervention.
Documentation and Follow-up
Proper documentation of head-to-toe assessments is essential for continuity of care and legal protection. Documentation should be:
- Objective and factual
- Complete and accurate
- Timely and legible
- Organized systematically
Follow-up assessments should be performed based on patient acuity, physician orders, and facility policies. Changes from baseline should be reported promptly to the healthcare team.
Conclusion
Head-to-toe assessment is a fundamental nursing skill that requires practice, knowledge, and systematic approach. It serves as the foundation for identifying patient problems, planning appropriate interventions, and evaluating patient outcomes. Regular practice and continued education help nurses maintain proficiency in this essential skill, ultimately improving patient care quality and safety.
The systematic approach outlined in this guide provides a framework for conducting thorough, efficient assessments while ensuring no important findings are overlooked. Remember that assessment is an ongoing process that requires critical thinking, clinical judgment, and effective communication with the healthcare team.
References
- Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2023). Seidel’s guide to physical examination: An interprofessional approach (10th ed.). Elsevier.
- Bickley, L. S., & Szilagyi, P. G. (2021). Bates’ guide to physical examination and history taking (13th ed.). Wolters Kluwer.
- Douglas, C., Windsor, C., & Lewis, P. (2021). Too much knowledge for a nurse? Use of physical assessment by final-semester nursing students. Nursing & Health Sciences, 23(2), 375-384. https://doi.org/10.1111/nhs.12828
- Giddens, J. F. (2020). Concepts for nursing practice (3rd ed.). Elsevier.
- Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2021). Medical-surgical nursing: Concepts for interprofessional collaborative care (10th ed.). Elsevier.
- Jarvis, C., & Eckhardt, A. (2024). Physical examination and health assessment (9th ed.). Elsevier.
- Jensen, S. (2023). Nursing health assessment: A best practice approach (4th ed.). Wolters Kluwer.
- Kee, J. L., Hayes, E. R., & Marshall, K. (2021). Pharmacology: A patient-centered nursing process approach (9th ed.). Elsevier.
- LeMone, P., Burke, K., Dwyer, T., Levett-Jones, T., Moxham, L., & Reid-Searl, K. (2020). Medical-surgical nursing: Critical thinking for person-centred care (4th ed.). Pearson Australia.
- Lewis, S. L., Bucher, L., Heitkemper, M. M., & Harding, M. M. (2022). Medical-surgical nursing: Assessment and management of clinical problems (11th ed.). Elsevier.
- Nursing and Midwifery Board of Australia. (2020). Registered nurse standards for practice. Australian Health Practitioner Regulation Agency.
- Potter, P. A., Perry, A. G., Stockert, P. A., & Hall, A. M. (2021). Fundamentals of nursing (10th ed.). Elsevier.
- Rosenberg, S., Hayes, K., McIlvennan, C., Kutner, J., Sacco, M., Kamal, A., & Bull, J. (2021). Nursing assessment and management of patients with heart failure. American Journal of Nursing, 121(6), 24-35. https://doi.org/10.1097/01.NAJ.0000753468.06376.93
- Silvestri, L. A. (2022). Saunders comprehensive review for the NCLEX-RN examination (9th ed.). Elsevier.
- Taylor, C., Lynn, P., & Bartlett, J. L. (2023). Fundamentals of nursing: The art and science of person-centered care (9th ed.). Wolters Kluwer.
- Treas, L. S., Wilkinson, J. M., Barnett, K. L., & Smith, M. H. (2021). Basic nursing: Concepts, skills, and reasoning (2nd ed.). F.A. Davis.
- Videbeck, S. L. (2020). Psychiatric-mental health nursing (8th ed.). Wolters Kluwer.
- Weber, J. R., & Kelley, J. H. (2022). Health assessment in nursing (7th ed.). Wolters Kluwer.
- Wilson, S. F., & Giddens, J. F. (2021). Health assessment for nursing practice (7th ed.). Elsevier.
- Wiseman, T., Rasmussen, B., Cullen, L., Stasa, H., Smyth, W., Noble, D., & Hutchinson, A. M. (2024). The impact of whole of patient nursing assessment frameworks on hospital inpatients: A scoping literature review. Journal of Advanced Nursing, 80(4), 1458-1471. https://doi.org/10.1111/jan.16025
Professional Guidelines and Resources
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association.
- International Council of Nurses. (2020). Guidelines on advanced practice nursing. International Council of Nurses.
- National Academy of Medicine. (2021). The future of nursing 2020-2030: Charting a path to achieve health equity. The National Academies Press.
- The Joint Commission. (2023). National patient safety goals. The Joint Commission Resources.
- World Health Organization. (2020). State of the world’s nursing 2020: Investing in education, jobs and leadership. World Health Organization.
Online Resources and Tools
- Harding, M. M., Kwong, J., Roberts, D., Hagler, D., & Reinisch, C. (2020). Lewis’s medical-surgical nursing: Assessment and management of clinical problems. Nursing Center. Retrieved from https://www.nursingcenter.com
- National Institute for Health and Care Excellence. (2022). Clinical assessment and diagnosis guidelines. NICE.
- Nurseslabs. (2024). Head-to-toe assessment: Complete physical assessment guide. Retrieved from https://nurseslabs.com/head-to-toe-assessment-complete-physical-assessment-guide/
- Simple Nursing. (2024). Head-to-toe assessment checklist for nursing with examples. Retrieved from https://simplenursing.com/how-to-conduct-head-to-toe-nurse-assessment/
- U.S. Department of Health and Human Services, Office of Inspector General. (2022). Hospital compliance with CMS patient safety reporting requirements. OIG Publications.

Dan Palmer is a dedicated academic writing specialist with extensive experience supporting nursing students throughout their educational journey. Understanding the unique challenges faced by nursing students who balance demanding clinical rotations, family responsibilities, and rigorous coursework, Dan provides professional assignment assistance that helps students maintain academic excellence without compromising their other commitments.
With a comprehensive understanding of nursing curriculum requirements and academic standards, Dan delivers high-quality, thoroughly researched assignments that serve as valuable learning resources. His expertise spans various nursing disciplines, including clinical practice, healthcare ethics, patient care management, and evidence-based research.
Dan’s approach combines meticulous attention to detail with a commitment to timely delivery, ensuring that busy nursing students receive the support they need when they need it most. His professional assistance has helped countless nursing students successfully navigate their academic programs while maintaining their professional and personal responsibilities.
Committed to academic integrity and excellence, Dan Palmer continues to be a trusted resource for nursing students seeking reliable, professional assignment support.

