Healthcare finance has changed drastically since 1950. Please discuss the changes that have occurred and the effect on healthcare delivery
Healthcare finance has changed drastically since 1950. Please discuss the changes that have occurred and the effect on healthcare delivery
Module 1: Assignment
Remember to submit your work following the file naming convention FirstInitial.LastName_M01.docx. For example, J.Smith_M01.docx. Remember that it is not necessary to manually type in the file extension; it will automatically append.
Start by reading and following these instructions:
- Quickly skim the questions or assignment below and the assignment rubric to help you focus.
- Read the required chapter(s) of the textbook and any additional recommended resources. Some answers may require you to do additional research on the Internet or in other reference sources. Choose your sources carefully.
- Consider the discussion and the any insights you gained from it.
- Create your Assignment submission and be sure to cite your sources, use APA style as required, check your spelling.
Assignment:
The History of Healthcare Finance. Write a 2000-2500 word essay addressing each of the following points/questions. Support your ideas with at least three (3) scholarly citations in your essay. Use strict APA guidelines to format the paper. The cover page and reference page do not count towards the minimum word amount and an abstract and table of contents are not necessary and if included are not part of the overall word count.
- Healthcare finance has changed drastically since 1950. Please discuss the changes that have occurred and the effect on healthcare delivery with each change.
Expert Answer and Explanation
The History of Healthcare Finance
The US healthcare finance has experienced many changes over the past seventy years. Papanicolas et al. (2018) noted that rapid advances in medical technology and science, budget-busting increases in health care expenditures fueled by public and private insurance, and substantial gains in health outcomes attributable to medical care have marked the financial changes in the US healthcare system in the past seven decades.
As the country struggles to get out of a multiyear economic and financial crisis, the public and policymakers have increasingly in on healthcare expenditures that are rising sharply (Waxman, 2012). In other words, since 1950, US healthcare finance has changed drastically regarding payment sources and objects of expenditure. This purpose has discussed the changes that have occurred in US healthcare finance since 1950 and how they have impacted healthcare delivery.
In the 1950s, various changes in US healthcare affected healthcare finance. For instance, the Revenue Act of 1954 excluded employers’ contributions to workers’ health plans from taxable income (Permanyer & Scholl, 2019). This law impacted healthcare delivery by ensuring that employees received various health services. In 1956, the military program was enacted to provide health insurance to family members of officers of the Armed forces. The change improved the accessibility of care to family members of Armed forces officers.
The 1960s marked a huge milestone in US healthcare finance. In 1960, the Federal Employees Health Benefits Plan (FEHBP) was formed to provide health insurance for federal workers (Permanyer & Scholl, 2019). This law improved federal workers’ access to care by reducing the cost of care. In 1965, President Johnson passed the Medicare and Medicaid programs and signed them into law, with Truman on his side. The two programs marked a fundamental healthcare finance change in the American healthcare system.
Medicare Part A was designed to pay for home health care, limited skilled nursing, and hospital care. Optional Medicare Part B was to support paying for physician care. Medicaid was a separate program. It was designed to help states cover healthcare services for long-term care, the disabled, and people from poor classes (Waxman, 2012). Medicare was developed for people aged 65 years and above, people with End-Stage Renal Disease, and certain younger people with disabilities. The program pays for hospital and medical costs.
Medicare Part A helps pay for a limited time at a skilled nursing facility after a hospital stay. This part also pays for some hospice and home health care (Malekinejad et al., 2018). Part B helps eligible people pay for services from care providers such as doctors, home health care, outpatient care, preventive services, and durable medical equipment. The program may also cover the cost of hearing, health and wellness programs, and dental care. It also pays for prescribed drugs.
Medicaid was developed to provide health coverage to some people with limited resources and income. This program is run by states with the help of the federal government. The mandatory benefits the federal government requires states to provide include physician services, inpatient and outpatient hospital services, home health services, and laboratory and x-ray services, among others (Waxman, 2012). Optional benefits include case management, prescription drugs, occupational therapy, and physical therapy.
The Medicare and Medicaid programs impacted healthcare finance by ensuring that older people aged 65 years and above, people with disabilities, individuals with End-Stage Renal Disease, and those with limited resources and finance access care at an affordable cost. Medicaid covers over 70 million American citizens today, and in 2014, it reimbursed about 50% of all hospitals’ medical expenses. The Congressional Budget Office forecasts that Medicare and Medicaid programs will survive indefinitely due to sweeping spending reforms that have been made.
The Medicaid program was amended in 1967 to include additional services to the program. The amendment allowed the program to provide insurance coverage to Americans not receiving cash assistance. The amendment also added Early and Periodic Screening and Diagnostic Testing (EPSDT) to the program. In 1972, Supplemental Security Income (SSI) program was created. The program was created to provide monthly payments to children and adults with disabilities whose resources or income are below federal financial limits.
The program also provided financial assistance to older people aged 65 and above without disabilities who meet the financial qualifications. This program impacted healthcare finance by providing older people and individuals with disabilities who are below the poverty line with the ability to access healthcare services at an affordable cost.
The program pays for the care costs of people who meet eligibility criteria. Two years later, Hawaii Prepaid Health Care Act was passed. This act required employers in Hawaii to cover any worker working for them for more than 20 hours a week. The law was amended in 1989 when the State Health Insurance Program was added to cover people not eligible for employer-based insurance or Medicaid. This law changed healthcare finance in Hawaii by allowing people who do not qualify for employer-based insurance or Medicaid to receive care funded by the state government.
In 1977, the Health Care Financing Administration (HCFA) was developed within the Department of Health, Education, and Welfare (HEW). The program was created to manage the federal government’s largest healthcare financing programs, evaluate authority, and exercise regulations designed to assure the quality of healthcare services for many people in the US. The program administers Medicare programs that buy medical care for 39 million disabled and elderly individuals. It also provides a Medicaid program operating jointly under the state and federal authority to offer care services to 33 million low-income people.
The creation of HCF ensured that federal and state authorities assign funds for Medicaid and Medicare to one organization, ensuring that the money is distributed properly. The change made it easy to get Medicaid and Medicare complaints. In 1980, the HEW was named the Department of Health and Human Services (DHHS). The Department of Education was separated from the DHHS, and the funds allocated to the DHHS were meant for health only. During the same year, the federal government provided federal funding to states to improve care and adoption assistance. This move ensured state governments had enough funds to support state-sponsored healthcare programs.
In 1983, Diagnostic Related Groups (DRGs) were introduced by Medicare as a payment system for hospital payments. This initiative improved healthcare finance by making it easy for hospitals to determine payor reimbursement rates and better control hospital costs by categorizing patients with similar clinical diagnoses. Emergency Medical Treatment and Active Labor Act (EMTALA) was enacted in 1986. This law greatly impacted healthcare finance, especially in the emergency department. The law requires hospitals in partnership with Medicate to screen and provide emergency treatment to all who come into their emergency rooms, even if they cannot pay.
The same year, Consolidated Omnibus Budget Reconciliation Act (COBRA) was enacted. This law changed healthcare finance by allowing workers who have lost their jobs to continue enjoying their health insurance plan for 18 months. Therefore, workers who have lost their jobs must not worry about their health and finances for one and a half years. Another vital law was created in the 1980s. The law is the Medicare Catastrophic Coverage Act (MCCA). MCCA was enacted in 1988. The law expanded Medicare coverage to include a cap on beneficiaries’ out-of-pocket expenses and prescription drugs.
In 1996, the Health Insurance Portability and Accountability Act (HIPAA). The law protects US workers by permitting them to carry their health insurance policies from employment to employment (Edemekong et al., 2018). It also allows employees to lose coverage and adjust to changes such as adoptions, births, and marriages by applying to a select group of health insurance plans. The law also blocks insurers from discriminating against people applying for plans because of health problems. The Mental Health Parity Act was enacted in the same year. The law improved health coverage for patients with mental health problems.
Personal Responsibility and Work Opportunity Act was also enacted in the same year. This law allowed the state governments to provide health coverage to children and parents at present Aid to Families with Dependent Children (AFDC) levels and higher. The law prohibited Medicaid from providing cover to legal immigrants within the first five years in the US, except when they need emergency care.
The State Children’s Health Insurance Program (S-CHIP) act was enacted as part of the Balanced Budget Act (BBA) in 1997. The law provided block grants to states allowing them to provide health coverage to low-income children above Medicaid eligibility levels. The law also allowed states to cover the health services of disabled workers whose incomes are up to 250% of the poverty level.
The Breast and Cervical Cancer Treatment and Prevention Act of 2000 expanded the Medicaid program. It allowed it to provide coverage to uninsured women who are receiving treatment for cervical or breast cancer if they have been diagnosed following the Center for Disease Control (CDC) screening program, regardless of resources or income. In 2003, the Medicare Prescription Drug Improvement and Modernization Act was enacted.
Pakizegee and Stefanacci (2018) noted that the act is the most significant expansion of Medicare since it was enacted. This low included prescription drug benefits. It mandated Medicare to provide cover for prescription drugs. The State of Massachusetts passed legislation to offer healthcare coverage to nearly all its residents in 2006.
The law needed the residents of Massachusetts to attain health insurance coverage and called for shared responsibility among employers, individuals, and the government in financing the expanded health coverage program. The program cut the uninsured rate by half within two years of its implementation.
In the same year, the City of San Francisco created the Healthy San Francisco program, which provided universal care to city residents. Mental Health Parity Act was amended in 2008. It required insurance companies to treat mental health problems, including alcohol and substance abuse disorders equality and physical problems when health policies cover both.
The last grand change in healthcare finance is the Affordable Care Act (ACA). This act greatly changed healthcare finance in the US. This law was a modified version of the all-inclusive coverage US presidents in the 1900s imagined. The act aimed to provide health insurance to the majority of US citizens. The act needs most Americans to apply for health insurance coverage. Individuals who have not applied for cover will be penalized. However, few protected groups are exempted from the penalty.
Companies that employ more than 200 employers are bound to offer their workers’ health insurance coverage under the law (Zhao et al., 2020). The act created the American Health Benefits Exchange allowing Americans to review and compare health insurance plans to identify the best plan. The act also provides healthcare professionals the opportunity to take parting in improving the delivery of care.
According to Zhao et al. (2020), the healthcare industry can benefit from programs that deliver effective and efficient services to the growing patient population while decreasing care expenses. The ACA led to the creation of accountable care organizations (ACOs). This value-based care program requires healthcare professionals to pay for the quality of care provided instead of quantity (Zhao et al., 2020). ACOs coordinate care for patients who have a specific health insurance program.
Conclusion
The US healthcare system has experienced a lot of changes in terms of healthcare finance since 1950. The first change was the Revenue Act of 1954 was enacted to exclude employers’ contributions to workers’ health plans from taxable income. The second important change was the creation of the Medicare and Medicaid programs. The two programs marked a fundamental healthcare finance change in the American healthcare system. The two programs provide health insurance coverage to more than 70 million Americans.
The HIPAA is another major healthcare reform that impacted health finance. The law protects US workers by permitting them to carry their health insurance policies from employment to employment. The ACA is recent major healthcare reform that impacted healthcare finance in the US. The act aimed to provide health insurance to the majority of US citizens. The act needs most Americans to apply for health insurance coverage. Individuals who have not applied for cover will be penalized.
References
Edemekong, P. F., Annamaraju, P., & Haydel, M. J. (2018). Health insurance portability and accountability act.
Malekinejad, M., Horvath, H., Snyder, H., & Brindis, C. D. (2018). The discordance between evidence and health policy in the United States: The science of translational research and the critical role of diverse stakeholders. Health Research Policy and Systems, 16(1), 1-21.
Monica Hendrix, M. J. (2019). Getting Health Care Costs Under Control While Improving Quality of Care: The Maryland Way. Journal of Health Care Finance.
Pakizegee, M., & Stefanacci, R. G. (2018). Value-based clinical pathways in the world of reference-priced Medicare Part B drugs. J Clin Pathways, 4(10), 38-39.
Papanicolas, I., Woskie, L. R., & Jha, A. K. (2018). Health care spending in the United States and other high-income countries. Jama, 319(10), 1024-1039.
Permanyer, I., & Scholl, N. (2019). Global trends in lifespan inequality: 1950-2015. PloS one, 14(5), e0215742.
Waxman, T. (2012). Financial and Business Management for the Doctor of Nursing Practice. Springer Publishing Co.
Zhao, J., Mao, Z., Fedewa, S. A., Nogueira, L., Yabroff, K. R., Jemal, A., & Han, X. (2020). The Affordable Care Act and access to care across the cancer control continuum: A review at 10 years. CA: A Cancer Journal For Clinicians, 70(3), 165-181.
Do You Want Original Paper Written From Scratch For Similar Assignment? Click Here To Place Your Order Use Coupon Code: NEW30 to Get 30% OFF Your First Order
Use Coupon Code: NEW30 to Get 30% OFF Your First Order
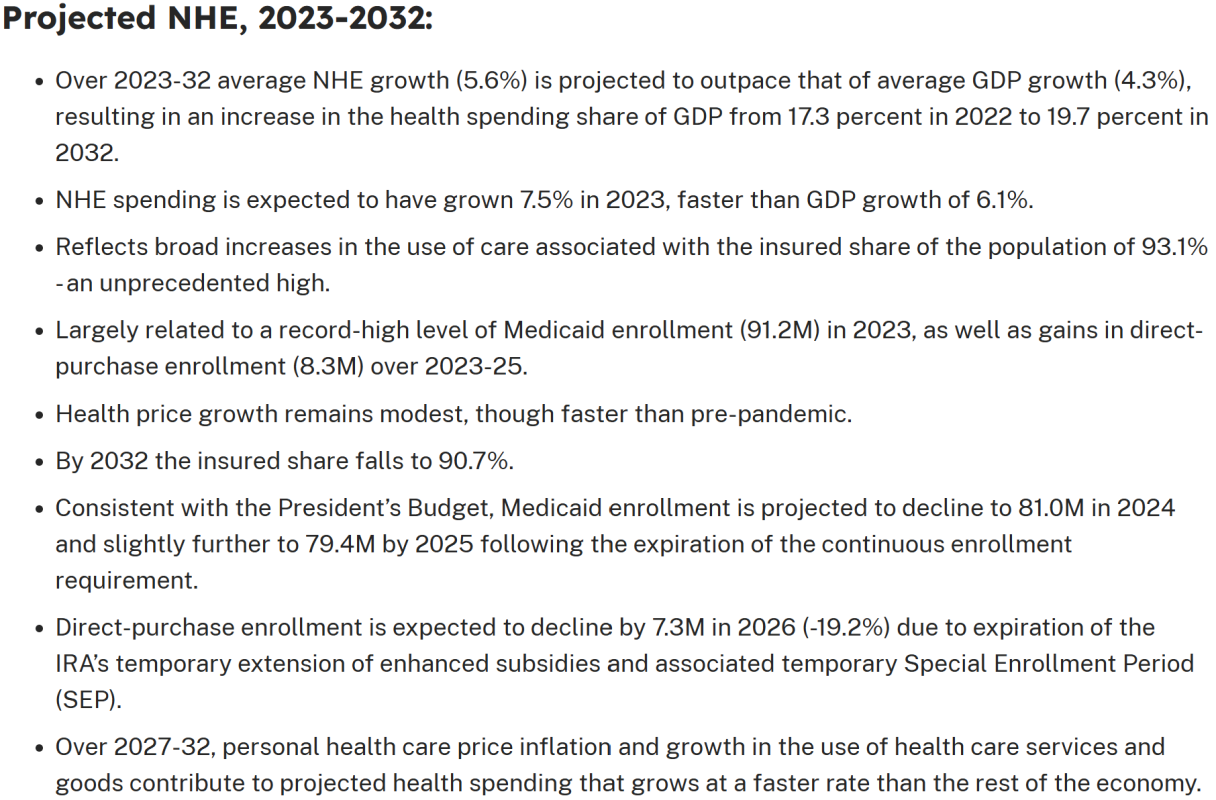
Major Trends in the U.S. Health Economy Since 1950
Introduction
The United States health economy has undergone profound transformations since 1950, evolving from a relatively simple system of individual practitioners and community hospitals to a complex, technology-driven ecosystem that now represents nearly one-fifth of the nation’s gross domestic product. The health care delivery system, which encompasses all medical services and activities that directly or indirectly impact patient care from institutional and individual medical providers, has been central to these changes (Dovetail, 2023). Understanding the health care delivery system definition is crucial for comprehending how structural changes have shaped economic trends over the past seven decades.
The Evolution of Health Care Delivery Systems
Defining the Modern Health Care Delivery System
The health care delivery system definition has evolved significantly since 1950. According to contemporary analysis, a health care delivery system refers to the formal arrangements and systems put in place to provide health care services to specific populations, encompassing the various actors and components involved in delivering health care (ScienceDirect, 2024). However, as noted by the National Academy of Sciences, while the phrase “health care delivery system” suggests order, integration, and accountability, these characteristics do not always exist in practice (National Academies Press, 2024).
The modern health care delivery system comprises four fundamental components: providers (hospitals, physicians, and other healthcare professionals), payers (insurance companies, government programs), patients (consumers of healthcare services), and regulatory bodies that oversee quality and access standards. This complex interplay has created what the International Society for Pharmacoeconomics and Outcomes Research describes as “one of the most complex healthcare systems in the world, formed by intertwining relationships between providers, payers, and patients receiving care” (ISPOR, 2024).
Major Economic Trends Since 1950
Explosive Growth in Health Care Spending
The most dramatic trend in the U.S. health economy since 1950 has been the exponential growth in healthcare expenditures. From representing approximately 4% of GDP in 1950, healthcare spending has grown to dominate the American economy. Recent data indicates that health spending represented 17.6% of GDP in 2023, similar to pre-pandemic shares after temporary increases during COVID-19 (American Medical Association, 2025).
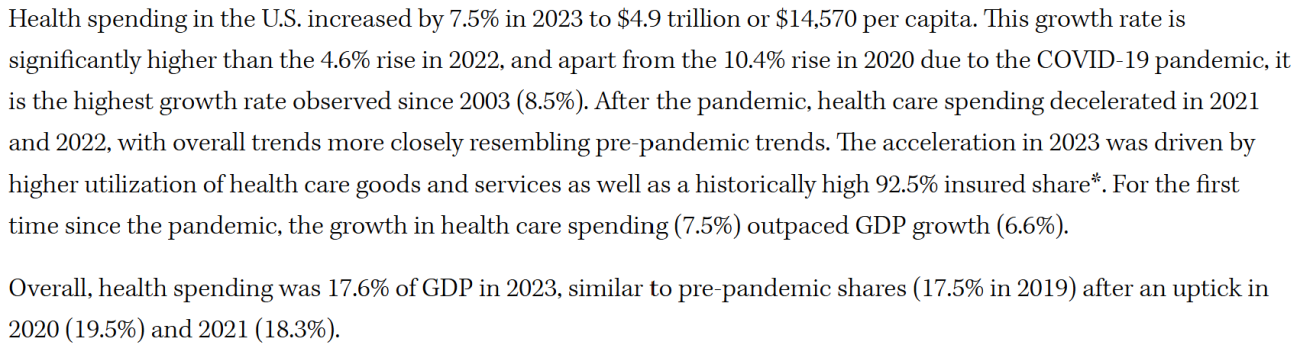
Source: American Medical Association
This growth trajectory shows no signs of abating. Healthcare industry economics are shifting toward non-acute care delivery, healthcare software, data, analytics, and specialty pharmacy segments, with McKinsey estimating that healthcare EBITDA will increase at a 7% compound annual growth rate to $987 billion in 2028 from a baseline of $676 billion in 2023 (McKinsey, 2025).
The Digital Transformation Revolution
One of the most significant contemporary trends reshaping the health care delivery system is digital transformation. Accelerated digital transformation has been cited as the issue most likely to impact global health systems in 2025, particularly notable given that healthcare has lagged years behind other industries such as retail and finance in adopting digital technologies (Deloitte, 2025).
This digital revolution encompasses telemedicine, electronic health records, artificial intelligence applications, and data analytics platforms that are fundamentally altering how care is delivered and paid for within the health care delivery system.
Employer Health Care Cost Pressures
The burden on U.S. employers continues to intensify, with healthcare spending projected to jump by nearly 8% in 2025, representing the largest annual increase in more than a decade (Cigna, 2025). This trend reflects broader systemic pressures within the health care delivery system, as plan sponsors increasingly focus on improving efficiency and eliminating waste to manage rising costs.
Comparative International Performance
Despite substantial investments, the U.S. health care delivery system continues to underperform relative to other developed nations. Analysis by the Commonwealth Fund reveals that Americans are living shorter, unhealthier lives while the United States outspends other wealthy nations on healthcare (Commonwealth Fund, 2020). In 2023, the U.S. saw a 5.4% increase in per capita health spending, a larger increase than most comparable nations (Peterson-KFF Health System Tracker, 2025).
Structural Changes in Care Delivery
Shift from Acute to Non-Acute Care
The health care delivery system has experienced a fundamental shift in focus from acute, hospital-based care toward community-based and preventive services. This transformation reflects both demographic changes, including an aging population, and evolving medical understanding of chronic disease management and prevention.
Workforce Challenges and Shortages
The health care delivery system faces significant workforce challenges that have economic implications. The United States expects a shortfall of up to 49,300 primary care physicians by 2030 and up to 52,000 primary care physicians by 2025, exacerbated by rising student debt and declining interest in primary care specialties (Annals of Internal Medicine, 2020).
Integration and Consolidation
The health care delivery system has witnessed unprecedented consolidation, with hospital systems, physician practices, and insurance companies merging to achieve economies of scale and improve care coordination. This trend has significant implications for market competition and healthcare pricing.
Policy and Regulatory Evolution
Medicare and Medicaid Impact
The introduction of Medicare and Medicaid in 1965 fundamentally altered the economics of the health care delivery system, creating government-sponsored healthcare coverage that now serves as a cornerstone of American healthcare financing. Recent projections indicate that Medicaid enrollment is expected to decline to 81.0 million in 2024 and 79.4 million by 2025 following the expiration of continuous enrollment requirements (CMS, 2024).
The Affordable Care Act Era
The Affordable Care Act (ACA) of 2010 represented another watershed moment in the evolution of the health care delivery system, expanding coverage while introducing new payment models and quality metrics that continue to shape the economic landscape.
Contemporary Challenges and Future Outlook
COVID-19 Pandemic Impact
The COVID-19 pandemic created unprecedented disruption within the health care delivery system, with health care spending rising rapidly in nearly all countries as governments sought to mitigate disease spread through testing, vaccination, and treatment programs (Commonwealth Fund, 2023). The pandemic accelerated many existing trends, particularly digital transformation and the shift toward value-based care models.
Emerging Technologies and Innovation
The health care delivery system continues to evolve with emerging technologies including artificial intelligence, precision medicine, and advanced therapeutics. These innovations promise to improve outcomes while potentially reducing costs, though they also require significant capital investments and workforce retraining.
Sustainability Concerns
The long-term sustainability of current spending trends remains a critical concern. With healthcare costs consistently outpacing general economic growth, policymakers, employers, and health system leaders are increasingly focused on identifying strategies to improve efficiency and value within the health care delivery system.
Conclusion
The transformation of the U.S. health economy since 1950 reflects the complex interplay of technological advancement, demographic change, policy intervention, and market forces. The health care delivery system has evolved from a relatively simple framework of individual practitioners and community hospitals to a sophisticated, technology-enabled ecosystem that now dominates the American economy.
Understanding the health care delivery system definition and its evolution is essential for comprehending current economic trends and future challenges. As the system continues to grapple with rising costs, workforce shortages, quality concerns, and the need for greater integration and efficiency, the next decade will likely bring continued transformation in how healthcare is delivered, financed, and regulated.
The trends identified in recent research suggest that the health care delivery system will continue to evolve toward greater digitization, increased focus on value-based care, and enhanced integration between various stakeholders. Success in managing these transitions will require sustained collaboration between providers, payers, policymakers, and patients to ensure that the system serves the health and economic interests of all Americans.
References
American Medical Association. (2025, April 17). Trends in health care spending. https://www.ama-assn.org/about/ama-research/trends-health-care-spending
Annals of Internal Medicine. (2020). Envisioning a better U.S. health care system for all: Health care delivery and payment system reforms. Annals of Internal Medicine. https://www.acpjournals.org/doi/10.7326/M19-2407
Centers for Medicare & Medicaid Services. (2024). NHE fact sheet. https://www.cms.gov/data-research/statistics-trends-and-reports/national-health-expenditure-data/nhe-fact-sheet
Cigna. (2025). Top health care trends of 2025 and how they will impact U.S. employers. https://newsroom.cigna.com/top-health-care-trends-of-2025
Commonwealth Fund. (2020, January). U.S. health care from a global perspective, 2019: Higher spending, worse outcomes? https://www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019
Commonwealth Fund. (2023, January). U.S. health care from a global perspective, 2022: Accelerating spending, worsening outcomes. https://www.commonwealthfund.org/publications/issue-briefs/2023/jan/us-health-care-global-perspective-2022
Deloitte. (2025, January 29). 2025 global health care outlook. https://www2.deloitte.com/us/en/insights/industry/health-care/life-sciences-and-health-care-industry-outlooks/2025-global-health-care-executive-outlook.html
Dovetail. (2023, July 31). Guide to healthcare delivery systems in the United States. https://dovetail.com/patient-experience/delivery-systems-in-healthcare/
International Society for Pharmacoeconomics and Outcomes Research. (2024). US healthcare system overview-background. https://www.ispor.org/heor-resources/more-heor-resources/us-healthcare-system-overview/us-healthcare-system-overview-background-page-1
McKinsey & Company. (2025, January 10). What to expect in US healthcare in 2025 and beyond. https://www.mckinsey.com/industries/healthcare/our-insights/what-to-expect-in-us-healthcare-in-2025-and-beyond
National Academies Press. (2024). 5. The health care delivery system. https://nap.nationalacademies.org/read/10548/chapter/7
Peterson-KFF Health System Tracker. (2025, April 9). How does health spending in the U.S. compare to other countries? https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries/
ScienceDirect. (2024). Health care delivery system – an overview. https://www.sciencedirect.com/topics/social-sciences/health-care-delivery-system

Dan Palmer is a dedicated academic writing specialist with extensive experience supporting nursing students throughout their educational journey. Understanding the unique challenges faced by nursing students who balance demanding clinical rotations, family responsibilities, and rigorous coursework, Dan provides professional assignment assistance that helps students maintain academic excellence without compromising their other commitments.
With a comprehensive understanding of nursing curriculum requirements and academic standards, Dan delivers high-quality, thoroughly researched assignments that serve as valuable learning resources. His expertise spans various nursing disciplines, including clinical practice, healthcare ethics, patient care management, and evidence-based research.
Dan’s approach combines meticulous attention to detail with a commitment to timely delivery, ensuring that busy nursing students receive the support they need when they need it most. His professional assistance has helped countless nursing students successfully navigate their academic programs while maintaining their professional and personal responsibilities.
Committed to academic integrity and excellence, Dan Palmer continues to be a trusted resource for nursing students seeking reliable, professional assignment support.