Post a description of the national healthcare issue/stressor you selected for analysis, and explain how the healthcare issue/stressor
Post a description of the national healthcare issue/stressor you selected for analysis, and explain how the healthcare issue/stressor may impact your work setting.
Review of Current Healthcare Issues
If you were to ask 10 people what they believe to be the most significant issue facing healthcare today, you might get 10 different answers. Escalating costs? Regulation? Technology disruption? Social Determinant such as environment/community, education, access/quality to healthcare?
These and many other topics are worthy of discussion. Not surprisingly, much has been said in the research, within the profession, and in the news about these topics. Whether they are issues of finance, quality, workload, or outcomes, there is no shortage of changes to be addressed.
In this Discussion, you examine a national healthcare issue and consider how that issue may impact your work setting. You also analyze how your organization has responded to this issue.
To Prepare:
- Review the Resources and select one current national healthcare issue/stressor to focus on.
- Reflect on the current national healthcare issue/stressor you selected and think about how this issue/stressor may be addressed in your work setting.
By Day 3 of Week 1
Post a description of the national healthcare issue/stressor you selected for analysis, and explain how the healthcare issue/stressor may impact your work setting. Which social determinant(s) most affects this health issue? Then, describe how your health system work setting has responded to the healthcare issue/stressor, including a description of what changes may have been implemented. Be specific and provide examples.
Expert Answer and Explanation
Description of the Issue
My selected issue of analysis is the nursing shortage which is characterized by the lack of adequate nursing professionals, resulting to the difficulty meeting patients’ demand for nursing care. This issue is tied to various factors including the bulging population of seniors, which drives up demand considering the prevalence of chronic health disorders such as hypertension in this population. The United States’ nursing shortage issue is a concern because of its negative impacts (Costa & Friese, 2022).
It particularly increases nurses’ workload, a problem seen in clinical settings understaffed with nurses. With nurses working intensively due to the high workload, they experience burnout, resulting to loss of motivation to work. This in turn causes the surge in cases of medical errors considering that emotional and physical exhaustion that occurs when nurses work for longer hours.
Impact of the Issue
The access to educational opportunities and the family income status are some of the social determinants of health that influence nursing shortage. The former is seen in underserved communities which have limited educational institutions or facilities that offer nursing training. Conversely, children from households that earn below the minimum wage may struggle with financing their education, resulting to poor educational outcomes for this group (Van Merode, Groot, & Somers, 2024).
Effect of the SDOH
To attract and retain nurses, the system has introduced a wellness program tailored towards addressing issues related to burnout and the psychological impact of work-related concerns. Every month, nurses get time for mindful breaks each shift day as a way of promoting nurses’ mental wellbeing.
Interventions for Addressing the Issue
However, the hospital needs to make changes like introducing a remote patient monitoring system which essentially minimizes the need for nurses to physically monitor patients. Alternatively, it can use a virtual system that virtually collects data about patients, and relays this information to nurses to identify appropriate interventions for patients (Griffiths et al., 2021).
References
Costa, D. K., & Friese, C. R. (2022). Policy Strategies for Addressing Current Threats to the U.S. Nursing Workforce. The New England journal of medicine, 386(26), 2454–2456. https://doi.org/10.1056/NEJMp2202662.
Griffiths, P., Saville, C., Ball, J. E., Jones, J., Monks, T., & Safer Nursing Care Tool study team (2021). Beyond ratios – flexible and resilient nurse staffing options to deliver cost-effective hospital care and address staff shortages: A simulation and economic modelling study. International journal of nursing studies, 117, 103901. https://doi.org/10.1016/j.ijnurstu.2021.103901.
Van Merode, F., Groot, W., & Somers, M. (2024). Slack Is Needed to Solve the Shortage of Nurses. Healthcare (Basel, Switzerland), 12(2), 220. https://doi.org/10.3390/healthcare12020220.
Alternative Expert Answer and Explanation
The nursing shortage is one of the most critical national healthcare challenges, and it has been a chronic source of stress for healthcare facilities, even more so due to the COVID-19 pandemic. The shortage affects the quality of patient care, staff motivation, and working pressure in my healthcare organization. Nurses often receive more patients than required, which causes staff burnout, reduced job satisfaction, and poor quality of patient care (Perkins, 2021).
In this context, the shortage is seen to be shaped by social factors such as education, which determines the supply of nurses through graduates, and economic conditions that determine the attraction and retention of nurses in areas of need. Slonim (2023) has pointed out workforce problems such as shortage and turnover as significant barriers to healthcare systems across the country.
As a result of the nursing shortage, my healthcare system has taken measures to deal with it. For example, measures towards increasing retention comprise the provision of high wages, tuition fee reimbursement, and professional development opportunities (Perkins, 2021). Leadership has focused on providing support and has used transformational leadership approaches to increase staff motivation. In their article, Broome and Marshall (2021) define transformational leadership as one of the best practices for motivating and enabling teams to become more resilient during tough times.
Some of them include the provision of training to new nurses by experienced ones and the development of a flexible working shift schedule. Further, it has relationships with regional nursing schools to ensure that new entrants are sourced and provided with internships and preceptorship to foster their retention.
These measures have eased some of these pressures, but the shortage is still a chronic problem that requires more effort. The continuous assessment of the applied measures and the constant feedback from the staff make these measures relevant and sensitive to the existing needs.
References
Broome, M., & Marshall, E. S. (2021). Transformational leadership in nursing: From expert clinician to influential leader (3rd ed.). Springer.
Perkins, A. (2021). Nursing shortage: Consequences and solutions. Nursing Made Incredibly Easy, 19(5), 49-54. https://doi.org/10.1097/01.NME.0000767268.61806.d9Links to an external site.
Slonim, A. (2023). Top challenges facing healthcare: Back to basics. Physician Leadership Journal, 10(2), 12–14. https://doi.org/10.55834/plj.2064149664Links to an external site.
Place your order now for a similar assignment and get fast, cheap and best quality work written by our expert level assignment writers. Limited Offer: Get 30% OFF Your First Order
Limited Offer: Get 30% OFF Your First Order
The Nursing Shortage Crisis: Current Statistics, Projections, and Impact on Healthcare
The United States healthcare system faces an unprecedented nursing shortage that threatens patient care delivery and healthcare sustainability. This crisis has been decades in the making, with demographic shifts, educational capacity limitations, and workplace challenges converging to create a perfect storm in the nursing profession. Understanding the scope, causes, and implications of this shortage is crucial for addressing one of the most pressing national healthcare stressors of our time.
Current State of the Nursing Shortage
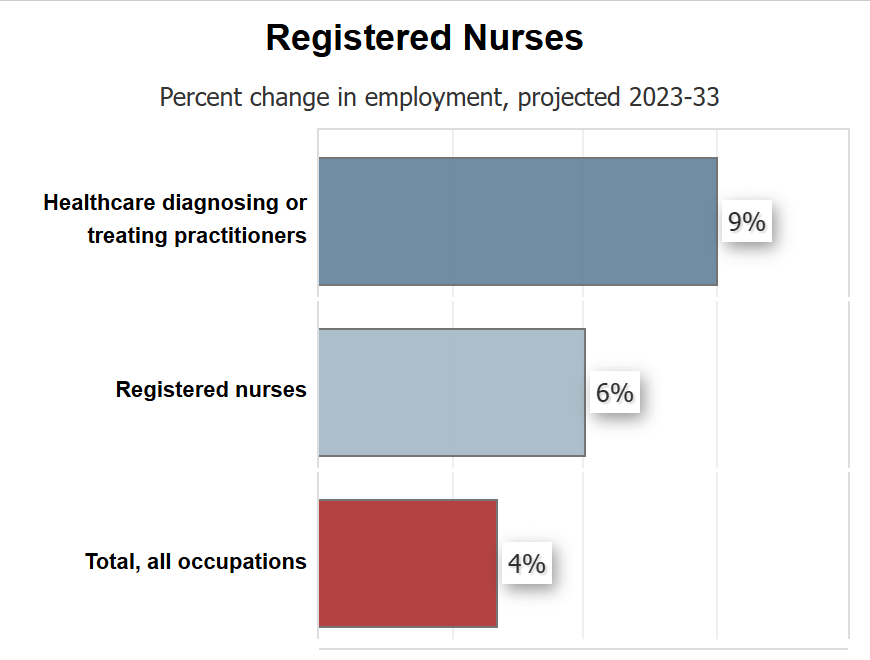
The nursing shortage represents one of the most significant workforce challenges in American healthcare. According to the U.S. Bureau of Labor Statistics, the nursing profession requires substantial growth to meet increasing demand. The U.S. Bureau of Labor Statistics projects that more than 275,000 additional nurses are needed from 2020 to 2030, and that employment opportunities for nurses will grow at 9 percent, faster than all other occupations (U.S. Department of Labor, 2022).
The magnitude of this shortage varies significantly across states and regions. The Bureau of Health Workforce projects that California will face the largest number of nursing shortages of any state, with a projected shortfall of 65,000 nurses by 2037 (University of St. Augustine for Health Sciences, 2024). California tops the list with an estimated 44,500 deficit in registered nurses, nearly three times the deficit in the next shortest state. Texas, New Jersey, and South Carolina will lack more than 10,000 RNs; Alaska, Georgia, and South Dakota will each be short several thousand (RegisteredNursing.org, 2025).
Projected Nursing Shortage by 2025 and Beyond
The projected nursing shortage by 2025 presents alarming statistics that underscore the urgency of this crisis. According to the 2020 HRSA Nurse Workforce Projections report, “Nationally, there is a projected shortage of 78,610 full-time equivalent (FTE) RNs in 2025 and a shortage of 63,720 FTE RNs in 2030.” This means that they’re predicting that 98% of the total demand for nurses will be met (Nurse.org, 2024).
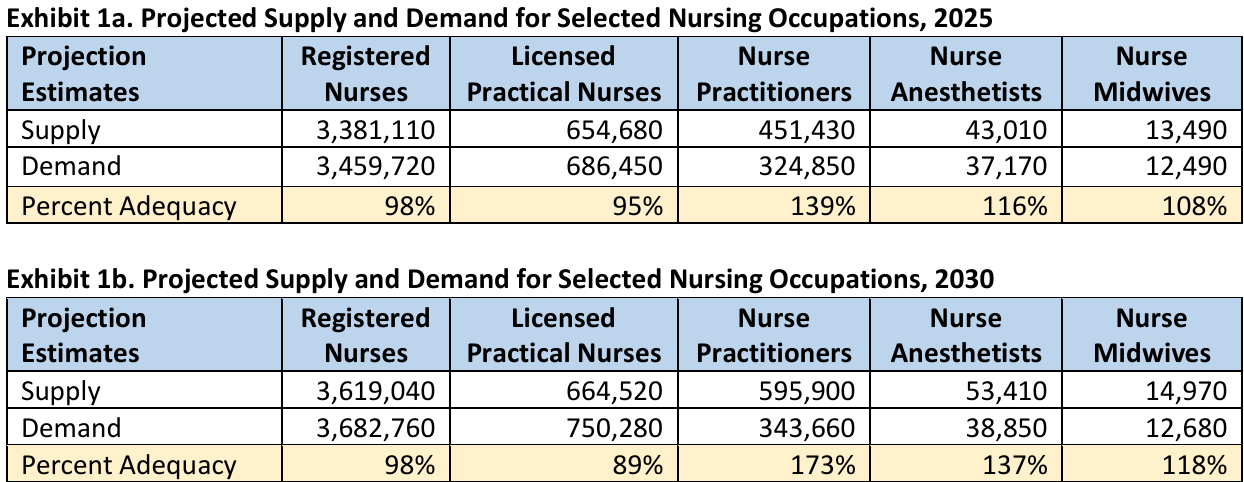
Source: HRSA
However, more recent data suggests the situation may be more severe than initially projected. According to the Health Resources and Services Administration (HRSA) Nurse Workforce Projections: 2026-2031 report issued in March 2024, the US is projected to see shortages of licensed practical nurses and registered nurses but not for the different specializations of nurse practitioners (Nightingale College, 2024).
The demographic reality driving these projections is particularly concerning. The US Bureau of Labor Statistics projects 194,500 average annual openings for registered nurses between 2020 and 2030, with employment projected to grow 9%. Accelerating Retirements—In 2020, the median age of RNs was 52 years with more than one-fifth indicating retirement intentions (American Nurses Association, 2017).
Causes of Nursing Shortages
Educational Capacity Limitations
One of the primary reasons for nurse shortage stems from the educational pipeline’s inability to meet demand. The U.S. is projected to experience a shortage of Registered Nurses (RNs) that is expected to intensify as Baby Boomers age and the need for health care grows. Compounding the problem is the fact that nursing schools across the country are struggling to expand capacity to meet the rising demand (American Association of Colleges of Nursing, 2024).
Demographic Shifts and Aging Population
The causes of nursing shortages are multifaceted and interconnected. The aging Baby Boomer generation represents a dual challenge: not only do they require more healthcare services as they age, but many nurses from this generation are also approaching retirement. This demographic shift creates increased demand while simultaneously reducing the available workforce.
Workplace Stressors and Burnout
Nursing shortages lead to errors, higher morbidity, and mortality rates. In hospitals with high patient-to-nurse ratios, nurses experience burnout, dissatisfaction, and the patients experienced higher mortality and failure-to-rescue rates than facilities with lower patient-to-nurse ratios (StatPearls, 2024).
The workplace environment has become increasingly challenging for nurses. “There is a lack of administrative support, tough working conditions and a lack of equipment,” she noted. “Health resource disparities, limited specialists and specialty care, and lower salaries in rural and underserved areas exacerbate the work conditions and increased risk of burnout” (Ohio University, 2025).
Pandemic Impact
The COVID-19 pandemic significantly accelerated the nursing shortage crisis. The data reveals that 100,000 nurses left the workforce during the pandemic and by 2027, almost 900,000, or almost one-fifth of 4.5 million total registered nurses, intend to leave the workforce, threatening the national health care system at large if solutions are not enacted (NCSBN, 2024).
Impact of Nursing Shortage on Nurses
The nursing shortage creates a vicious cycle that perpetuates itself through its impact on existing nurses. Frequent shortage of nursing in a healthcare system to provide services may lead to stress and burnout, which will affect nurse’s performance and increase the chances of medical errors, especially in patient’s treatment, clinical care and laboratory tests (PMC, 2023).
Physical and Emotional Exhaustion
The truth about nursing shortage reveals the profound toll it takes on healthcare workers. Overwhelmed frontline RNs confront a persistent risk of nurse burnout – a term that barely encompasses the profound physical and emotional exhaustion they face (University of St. Augustine for Health Sciences, 2024).
Research indicates that burnout among nurses is closely linked to working conditions and staffing levels. Research suggests nurses who work longer shifts and who experience sleep deprivation are likely to develop burnout. Others have reported a strong correlation between sleep deprivation and errors in the delivery of patient care. Emotional exhaustion has been identified as a major factor (PMC, 2021).
Career Satisfaction and Retention
The impact extends beyond individual nurses to affect overall career satisfaction and retention rates. When nurses are overworked and under-supported, they are more likely to leave the profession entirely, further exacerbating the shortage. This creates a dangerous cycle where remaining nurses face even greater workloads, leading to higher turnover rates.
National Healthcare Stressors and Systemic Implications
The nursing shortage represents one of the most significant national healthcare stressors, with implications that extend far beyond individual healthcare facilities. The shortage affects the entire healthcare delivery system, from emergency departments to long-term care facilities, and has profound implications for patient safety and healthcare quality.
Patient Safety Concerns
The shortage directly impacts patient safety through increased patient-to-nurse ratios, longer response times, and increased likelihood of medical errors. Healthcare facilities struggle to maintain safe staffing levels, often relying on temporary staffing solutions that may not provide the continuity of care that patients need.
Economic Impact
The economic implications of the nursing shortage are substantial. Healthcare facilities face increased costs related to recruitment, retention, overtime pay, and temporary staffing. The shortage also contributes to healthcare inefficiencies and potentially avoidable complications that increase overall healthcare costs.
Healthcare Access and Quality
In many regions, particularly rural and underserved areas, the nursing shortage contributes to reduced healthcare access. Some facilities may be forced to reduce services or close units entirely due to insufficient nursing staff, creating healthcare deserts that force patients to travel greater distances for care.
Conclusion
The nursing shortage crisis represents a complex challenge that requires immediate and sustained attention from policymakers, healthcare leaders, and educational institutions. The projected nursing shortage by 2025 and beyond, combined with the multiple factors contributing to this crisis, creates an urgent need for comprehensive solutions.
Addressing this shortage will require a multifaceted approach that includes expanding nursing education capacity, improving working conditions, enhancing compensation and benefits, and implementing policies that support nurse well-being and career satisfaction. The truth about nursing shortage is that it affects not just individual nurses but the entire healthcare system and the patients it serves.
The nursing shortage statistics paint a clear picture: without immediate action, the United States faces a healthcare workforce crisis that could compromise patient care quality and access for millions of Americans. The time for action is now, as the projected shortages will only worsen without coordinated efforts to address the underlying causes and support the nursing profession.
The stakes are high, and the consequences of inaction could be devastating for American healthcare. By understanding the full scope of this crisis and its implications, stakeholders can work together to develop and implement solutions that ensure a robust, sustainable nursing workforce for the future.
References
American Association of Colleges of Nursing. (2024). Nursing shortage fact sheet. https://www.aacnnursing.org/news-data/fact-sheets/nursing-shortage
American Nurses Association. (2017, October 14). The state of the nursing workforce. https://www.nursingworld.org/practice-policy/workforce/
National Council of State Boards of Nursing. (2024). NCSBN research projects significant nursing workforce shortages and crisis. https://www.ncsbn.org/news/ncsbn-research-projects-significant-nursing-workforce-shortages-and-crisis
Nightingale College. (2024). Nursing shortage: 2025 US statistics by state. https://nightingale.edu/blog/nursing-shortage-by-state.html
Nurse.org. (2024). Nursing shortage may be worse by state than projected, new analysis shows. https://nurse.org/education/nursing-shortage-by-state-analysis/
Ohio University. (2025, January 7). Nursing shortages: A threat to patient care. https://www.ohio.edu/news/2024/11/nursing-shortages-threat-patient-care
RegisteredNursing.org. (2025, February 12). The places with the largest nursing shortages. https://www.registerednursing.org/articles/largest-nursing-shortages/
StatPearls. (2024). Nursing shortage. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK493175/
U.S. Department of Labor. (2022, October 3). US Department of Labor announces $80M funding opportunity to help train, expand, diversify nursing workforce; address shortage of nurses. https://www.dol.gov/newsroom/releases/eta/eta20221003
University of St. Augustine for Health Sciences. (2024, December 30). Nursing shortage: A 2024 data study reveals key insights. https://www.usa.edu/blog/nursing-shortage/

Dan Palmer is a dedicated academic writing specialist with extensive experience supporting nursing students throughout their educational journey. Understanding the unique challenges faced by nursing students who balance demanding clinical rotations, family responsibilities, and rigorous coursework, Dan provides professional assignment assistance that helps students maintain academic excellence without compromising their other commitments.
With a comprehensive understanding of nursing curriculum requirements and academic standards, Dan delivers high-quality, thoroughly researched assignments that serve as valuable learning resources. His expertise spans various nursing disciplines, including clinical practice, healthcare ethics, patient care management, and evidence-based research.
Dan’s approach combines meticulous attention to detail with a commitment to timely delivery, ensuring that busy nursing students receive the support they need when they need it most. His professional assistance has helped countless nursing students successfully navigate their academic programs while maintaining their professional and personal responsibilities.
Committed to academic integrity and excellence, Dan Palmer continues to be a trusted resource for nursing students seeking reliable, professional assignment support.