Examine changes introduced to reform or restructure the US – Trends and Issues in Today’s Health Care (NRS-440VN)
Examine changes introduced to reform or restructure the U.S. health care delivery system.
Examine changes introduced to reform or restructure the U.S. health care delivery system. In a 1,000-1,250 word paper, discuss action taken for reform and restructuring and the role of the nurse within this changing environment.
Include the following:
- Outline a current or emerging health care law or federal regulation introduced within the last 5 years to reform or restructure some aspect of the health care delivery system. Describe the effect of this on nursing practice and the nurse’s role and responsibility.
- Discuss how quality measures and pay for performance affect patient outcomes. Explain how these affect nursing practice and describe the expectations and responsibilities of the nursing role in these situations.
- Discuss professional nursing leadership and management roles that have arisen and how they are important in responding to emerging trends and in the promotion of patient safety and quality care in diverse health care settings.
- Research emerging trends. Predict two ways in which the practice of nursing and nursing roles will grow or transform within the next five years in response to upcoming trends or predicted issues in health care.
You are required to cite a minimum of three sources to complete this assignment. Sources must be published within the last 5 years, appropriate for the assignment criteria, and relevant to nursing practice.
Prepare this assignment according to the guidelines found in the APA Style Guide, located in the Student Success Center.
This assignment uses a rubric. Please review the rubric prior to beginning the assignment to become familiar with the expectations for successful completion.
You are required to submit this assignment to LopesWrite. A link to the LopesWrite technical support articles is located in Class Resources if you need assistance.
Expert Answer and Explanation
U.S. Health Care Delivery System Reforms
The healthcare system is always undergoing changes from time to time. Different healthcare facilities have to abide to the set standards an ensure that they are in line with the set guidelines. The Congress and other third-party agencies are also invested in the delivery of appropriate and quality medical practice. As a result, constant reviews and amendments to care systems is a continuation process. Since the enactment of the Affordable Care Act in 2010, the majority of the US population has been able to access quality healthcare with ease.
Be that as it may, various committees were formed in the Trump era, leading to several modifications that received mixed reactions from different stakeholders. Some saw them as a threat to the healthcare and well-being of citizens and an attempt to undermine the Affordable Care Act. In the current legislature, different reforms are constantly being taken into account and restructuring put in place with changes in the overall care process.
Current Health Care Law
One of the most recent health care law formulations is the S.352 – Health Care Improvement Act of 2021 sponsored by Senator Warner, Mark R. [D-VA] (Introduced 02/22/2021) (Congress.gov, 2021). The bill is aimed at creating additional reforms to the existing Affordable Care Act of 2009 in various ways. For instance, the main aim of the bill is to ensure a reduction in the costs of working families (Congress.gov, 2021). The strategy is to further reduce the premiums that the families are paying as well as the out of pocket costs.
The strategy will see to it that the Health Human Services create a more affordable and low-cost option of the families. The strategy also seeks to eliminate the policy that prevents families making more than 400 percent of the federal poverty line to be provided with premium subsidy (Warner, 2021). The funds can be used to support the program to lower costs for the working families and reduce the overall cost. The bill also seeks to reduce the cost for working families by negotiating the cost of prescription drugs and lifting the ban against negotiation with pharmaceutical companies to lower the cost of medication.
The other aim of the proposed amendments includes an increase in health care enrollment or access to care (Warner, 2021). With a reduced number of the uninsured, the legislation will be creating a means to increase accessibility to quality medical care for low-income families and other that might be in need of the service. The legislation has a direct impact on nursing practice since it creates an avenue within which appropriate care can be administered for different settings (Warner, 2021).
The legislation will increase the number if patient accessing healthcare facility, and with it the need for nurses to care for an even larger number of patients. Nurses need to be prepared to deal with the diversity and also ensure access and quality of care to all patients.
Impact of Quality Measures and Pay for Performance on Patient Outcome
Quality measures and pay for performance programs are designed to improve patient outcomes by incentivizing healthcare providers to achieve certain performance goals. The use of quality measures and pay for performance programs can have a significant impact on patient outcomes, as well as on the nursing practice (Endeshaw, 2021).
For instance, the use of quality measures provide a defined set of standards that can be used by healthcare providers to ensure that patients receive high-quality care. These standards include protocols for appropriate screening, need for holistic care, and proper patient education (Endeshaw, 2021). On the other hand, Pay for performance programs link reimbursement to the achievement of healthcare goals (Mathes et al., 2019).
The use of quality measures and pay for performance programs can have a significant impact on patient outcomes (Endeshaw, 2021). By incentivizing healthcare providers to provide high-quality care, patients are more likely to receive timely and appropriate treatment, leading to improved health outcomes. Additionally, these programs can also improve patient safety, as healthcare providers are incentivized to reduce medical errors and adverse events.
Nurses are expected to be actively involved in quality improvement initiatives, such as implementing evidence-based practices and participating in performance improvement projects (Mathes et al., 2019). They are also responsible for monitoring and documenting patient outcomes to ensure that they are meeting the required standards.
Nurse Leadership and Management
Professional nursing leadership and management roles have become increasingly important in responding to emerging trends and promoting patient safety and quality care in diverse healthcare settings (Morse & Warshawsky, 2021). With the emerging trends requiring nurses to promote and ensure patient safety, the role of the nursing leadership ought to change to conform to the new reforms.
Nurse leaders are required to be open to change and ensure that the team accepts and adopts the changes to wards meeting the new dynamics. For instance, nurses are required to embrace to adoption of new technologies or practical changes based on the need to ensure patient safety (Morse & Warshawsky, 2021). New nursing roles have also arisen to help address the issues and further promote the attainment of quality care.
These nursing leadership and management roles are important in responding to emerging trends and promoting patient safety and quality care in diverse healthcare settings. For example, as healthcare becomes more complex and technology-driven, nurse managers must ensure that staff members have the necessary training and support to provide safe, effective care (Booth et al., 2021).
On the other hand, Chief Nursing Officers play a critical role in ensuring that nursing practice is aligned with the organization’s mission, vision, and values, and that patient care is always the top priority.
Emerging Trends and Future of Nursing
The field of nursing is constantly evolving to adapt to emerging trends in healthcare. In this regard, new technologies, and practices are being adopted to facilitate care delivery processes (Buchanan et al., 2020). Other trends in the nursing field include the increase in aging population, health disparities, population health and interprofessional collaboration.
These issues have an impact on the future of nursing and how it can be positioned in response to the different care needs (Thibault, 2020). To prepare for these emerging trends, the future of nursing will require a focus on education and professional development. Nurses will need to pursue advanced degrees, participate in continuing education programs, and engage in lifelong learning to stay up-to-date with the latest developments in healthcare.
Conclusion
Quality measures and pay for performance programs can have a significant impact on patient outcomes, as well as on the nursing practice. On the other hand, professional nursing leadership and management roles have become increasingly important in responding to emerging trends and promoting patient safety and quality care in diverse healthcare settings.
Overall, the future of nursing will require a continued commitment to excellence in patient care, education, and professional development, as well as a willingness to adapt to emerging trends and to be leaders in shaping the future of healthcare.
References
Booth, R. G., Strudwick, G., McBride, S., O’Connor, S., & López, A. L. S. (2021). How the nursing profession should adapt for a digital future. bmj, 373.
Buchanan, C., Howitt, M. L., Wilson, R., Booth, R. G., Risling, T., & Bamford, M. (2020). Predicted influences of artificial intelligence on the domains of nursing: scoping review. JMIR nursing, 3(1), e23939.
Congress.gov. (2021). Text – S.352 – 117th Congress (2021-2022): Health Care Improvement Act of 2021. Congress.gov. https://www.congress.gov/bill/117th-congress/senate-bill/352/text
Endeshaw, B. (2021). Healthcare service quality-measurement models: a review. Journal of Health Research, 35(2), 106-117.
Mathes, T., Pieper, D., Morche, J., Polus, S., Jaschinski, T., & Eikermann, M. (2019). Pay for performance for hospitals. Cochrane Database of Systematic Reviews, (7).
Morse, V., & Warshawsky, N. E. (2021). Nurse leader competencies: Today and tomorrow. Nursing administration quarterly, 45(1), 65-70.
Thibault, G. E. (2020). The future of health professions education: emerging trends in the United States. FASEB BioAdvances, 2(12), 685.
Warner, M., R. (2021). The Health Care Improvement Act of 2021. Senate.gov. https://www.warner.senate.gov/public/_cache/files/a/5/a58ea9eb-879d-43ba-9b5d-25a2b8571354/58BBEDF6DCB6898F674FA0561E8B683D.the-health-care-improvement-act.pdf
Place your order now for a similar assignment and get fast, cheap and best quality work written by our expert level assignment writers. Use Coupon Code: NEW30 to Get 30% OFF Your First Order
Use Coupon Code: NEW30 to Get 30% OFF Your First Order
Healthcare Delivery System Reforms in the United States: A Comprehensive Analysis of Recent Changes and Their Impact (2020-2025)
Abstract
The United States healthcare delivery system has undergone significant transformations in recent years, driven by legislative reforms, payment model innovations, and the ongoing need to address systemic issues of cost, quality, and access. This comprehensive analysis examines the key changes introduced to reform and restructure the U.S. healthcare delivery system between 2020 and 2025, evaluating their impact on healthcare outcomes, costs, and system performance. The analysis reveals both progress and persistent challenges in achieving a more efficient, equitable, and effective healthcare system.
Introduction
The United States healthcare system has long been characterized by high costs, variable quality, and significant disparities in access to care. Despite spending more per capita on healthcare than any other developed nation, the U.S. consistently ranks poorly in international comparisons of health system performance (Commonwealth Fund, 2024). Recent reform efforts have focused on transforming payment models, improving care coordination, and addressing structural inefficiencies that have plagued the system for decades.
Major Healthcare Delivery System Reforms (2020-2025)
Payment System Transformation
One of the most significant areas of reform has been the transformation of healthcare payment systems. The law has also begun the process of transforming health care payment systems, with an estimated 30% of traditional Medicare payments now flowing through alternative payment models like bundled payments or accountable care organizations (Commonwealth Fund, 2022). This shift from volume-based to value-based payment models represents a fundamental restructuring of healthcare financial incentives.
The adoption of alternative payment models (APMs) has accelerated significantly since 2020, with the Centers for Medicare & Medicaid Services (CMS) expanding various programs including:
- Accountable Care Organizations (ACOs)
- Bundled payment initiatives
- Merit-based Incentive Payment System (MIPS)
- Advanced Alternative Payment Models (Advanced APMs)
Healthcare Spending and Cost Trends
Healthcare expenditure continues to represent a significant portion of the U.S. economy. Health spending in the U.S. increased by 7.5% in 2023 to $4.9 trillion or $14,570 per capita (American Medical Association, 2025). This represents both the scale of the healthcare sector and the ongoing challenge of cost containment.
Future projections indicate continued growth in healthcare spending. We estimate that healthcare EBITDA will increase at a 7 percent CAGR to $987 billion in 2028 from a baseline of $676 billion in 2023 (McKinsey & Company, 2025).
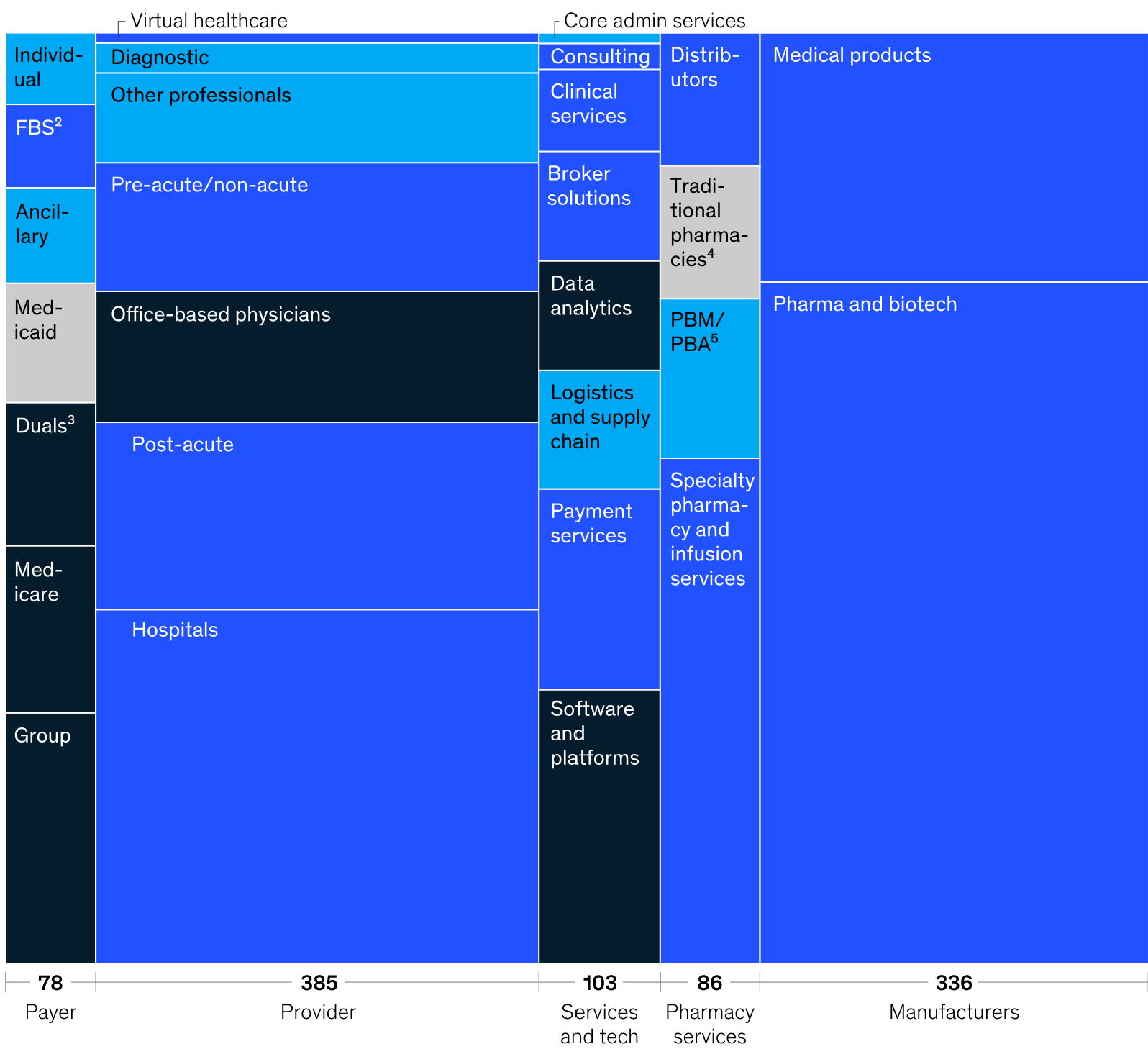
Source: McKinsey & Company
Delivery System Reform Initiatives
The Commonwealth Fund has identified key areas where delivery system reform is needed, emphasizing that we need to improve the way health care is organized, delivered, and paid for — particularly when it comes to people with high needs and high costs (Commonwealth Fund, 2025).
Impact of the Affordable Care Act Reforms
Payment and Delivery System Changes
The U.S. health care system has long been marked by high spending, comparatively poor health outcomes, inequities, waste, and inefficiency. To address these issues, the Affordable Care Act (ACA) includes several provisions to reform how the nation organizes, structures, and pays for its health care (Commonwealth Fund, 2022).
The ACA’s delivery system reforms have focused on several key areas:
- Care Coordination Improvements: Enhanced integration between primary care, specialty care, and social services
- Quality Measurement and Reporting: Implementation of standardized quality metrics across providers
- Prevention and Population Health: Emphasis on preventive care and community health initiatives
- Health Information Technology: Advancement of electronic health records and interoperability
Coverage and Access Improvements
Despite ongoing challenges, the ACA has made significant strides in expanding healthcare coverage. However, projected changes in enrollment patterns indicate evolving dynamics in coverage: Medicaid enrollment is projected to decline to 81.0M in 2024 and slightly further to 79.4M by 2025 following the expiration of the continuous enrollment requirement (Centers for Medicare & Medicaid Services, 2025).
Current Challenges and System Performance
International Comparisons
The 2024 Commonwealth Fund international health system performance study continues to highlight areas where the U.S. system lags behind other developed nations. In the U.S., the 2024 out-of-pocket limit for marketplace plans under the Affordable Care Act (ACA) cannot be more than $9,450 for single plans and $18,900 for family plans (Commonwealth Fund, 2024), which remains significantly higher than cost-sharing limits in comparable countries.
Trust and Public Confidence
Public trust in the healthcare system has experienced significant challenges. A Harvard/Northwestern poll showed that trust fell from 71.5% in April 2020 to 40.1% by January 2024 across all groups (Tucker, 2025), indicating a substantial erosion of confidence in healthcare institutions.
Workforce Challenges
The healthcare system faces significant workforce shortages, particularly in primary care. The United States expects a shortfall of up to 49,300 primary care physicians by 2030 and up to 52,000 primary care physicians by 2025 (Annals of Internal Medicine, 2020).
Key Reform Categories and Their Impacts
Table 1: Major Healthcare Delivery System Reform Categories (2020-2025)
| Reform Category | Key Initiatives | Primary Objectives | Measured Outcomes |
|---|---|---|---|
| Payment Reform | Alternative Payment Models, Value-Based Care | Cost reduction, quality improvement | 30% of Medicare payments through APMs |
| Care Coordination | ACOs, Medical Homes | Improved care integration | Reduced readmissions, better outcomes |
| Quality Improvement | MIPS, Quality Reporting | Standardized performance measurement | Enhanced transparency, accountability |
| Access Enhancement | Medicaid Expansion, Marketplace Subsidies | Coverage expansion | Reduced uninsured rates |
| Technology Integration | EHR Adoption, Interoperability | Information sharing, efficiency | Improved care coordination |
Table 2: Healthcare System Performance Indicators (2020-2025)
| Indicator | 2020 | 2023 | 2024 | 2025 (Projected) | Source |
|---|---|---|---|---|---|
| Total Healthcare Spending | $4.1 trillion | $4.9 trillion | – | – | AMA, 2025 |
| Per Capita Spending | $12,530 | $14,570 | – | – | AMA, 2025 |
| Medicare APM Participation | 25% | 30% | – | – | Commonwealth Fund, 2022 |
| Medicaid Enrollment | 85M | 83M | 81M | 79.4M | CMS, 2025 |
| Public Trust Level | 71.5% | – | 40.1% | – | Tucker, 2025 |
Future Directions and Recommendations
Structural Reforms Needed
Healthcare experts continue to advocate for fundamental structural changes to address persistent system challenges. The need for comprehensive reform remains urgent, with calls for policies that prioritize patient interests and improve care coordination across the continuum of care.
Technology and Innovation
The integration of advanced technologies, including artificial intelligence, telemedicine, and precision medicine, represents a significant opportunity for system improvement. These innovations have the potential to enhance care quality while reducing costs and improving access.
Workforce Development
Addressing the projected shortage of healthcare professionals, particularly in primary care, requires coordinated efforts in education, training, and retention. Policy interventions to support healthcare workforce development are essential for system sustainability.
Conclusion
The U.S. healthcare delivery system has undergone significant reforms between 2020 and 2025, with notable progress in payment model transformation, care coordination, and quality improvement initiatives. However, persistent challenges in cost containment, access equity, and system performance relative to international peers indicate that additional reforms are necessary.
The transition from volume-based to value-based payment models represents a fundamental shift in healthcare economics, with early evidence suggesting positive impacts on cost and quality outcomes. The expansion of alternative payment models, particularly through Medicare initiatives, has demonstrated the potential for system-wide transformation.
Despite these advances, the healthcare system continues to face significant challenges, including workforce shortages, declining public trust, and ongoing cost pressures. Future reform efforts must address these systemic issues while building upon the foundation of changes implemented in recent years.
The path forward requires continued commitment to evidence-based policy development, stakeholder engagement, and a focus on achieving the triple aim of improved population health, enhanced patient experience, and reduced per capita costs. Only through sustained reform efforts can the U.S. healthcare system achieve its potential to provide high-quality, accessible, and affordable care for all Americans.
References
American Medical Association. (2025, April 17). Trends in health care spending. AMA Research. https://www.ama-assn.org/about/ama-research/trends-health-care-spending
Annals of Internal Medicine. (2020). Envisioning a better U.S. health care system for all: Health care delivery and payment system reforms. https://www.acpjournals.org/doi/10.7326/M19-2407
Centers for Medicare & Medicaid Services. (2025). NHE fact sheet. National Health Expenditure Data. https://www.cms.gov/data-research/statistics-trends-and-reports/national-health-expenditure-data/nhe-fact-sheet
Commonwealth Fund. (2022, April). The impact of the payment and delivery system reforms of the Affordable Care Act. Commonwealth Fund Publications. https://www.commonwealthfund.org/publications/2022/apr/impact-payment-and-delivery-system-reforms-affordable-care-act
Commonwealth Fund. (2024, September). Mirror, mirror 2024: A portrait of the failing U.S. health system. Fund Reports. https://www.commonwealthfund.org/publications/fund-reports/2024/sep/mirror-mirror-2024
Commonwealth Fund. (2025). Delivery system reform. https://www.commonwealthfund.org/delivery-system-reform
McKinsey & Company. (2025, January 10). What to expect in US healthcare in 2025 and beyond. Healthcare Insights. https://www.mckinsey.com/industries/healthcare/our-insights/what-to-expect-in-us-healthcare-in-2025-and-beyond
Tucker, J. A. (2025, May 6). Small reforms to improve the US medical system. Capitalism Magazine. https://capitalismmagazine.com/2025/05/small-reforms-to-improve-the-us-medical-system/

Dan Palmer is a dedicated academic writing specialist with extensive experience supporting nursing students throughout their educational journey. Understanding the unique challenges faced by nursing students who balance demanding clinical rotations, family responsibilities, and rigorous coursework, Dan provides professional assignment assistance that helps students maintain academic excellence without compromising their other commitments.
With a comprehensive understanding of nursing curriculum requirements and academic standards, Dan delivers high-quality, thoroughly researched assignments that serve as valuable learning resources. His expertise spans various nursing disciplines, including clinical practice, healthcare ethics, patient care management, and evidence-based research.
Dan’s approach combines meticulous attention to detail with a commitment to timely delivery, ensuring that busy nursing students receive the support they need when they need it most. His professional assistance has helped countless nursing students successfully navigate their academic programs while maintaining their professional and personal responsibilities.
Committed to academic integrity and excellence, Dan Palmer continues to be a trusted resource for nursing students seeking reliable, professional assignment support.


